Dean T. Giacobbe, MD
- Anesthesiologist
- University Medical Center at Princeton
- Princeton, New Jersey
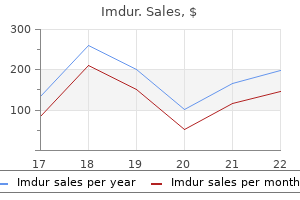
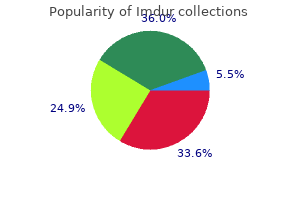
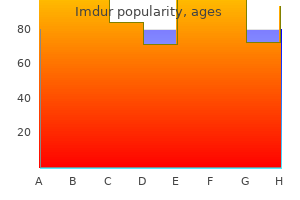
Lundstrom M pain treatment center lexington ky fax number order 40 mg imdur overnight delivery, Albrecht S sinus pain treatment natural buy imdur 40mg overnight delivery, Hakansson I pain treatment for gout purchase imdur 40mg fast delivery, Lorefors R neck pain treatment physiotherapy order imdur 40 mg without a prescription, Ohlsson S pain management in dogs cheap 40 mg imdur free shipping, Polland W pain treatment methadone purchase imdur with amex, Schmid A, Svensson G, Wendel E. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. The Cataract National Dataset electronic multi-centre audit of 55,567 operations: updating benchmark standards of care in the United Kingdom and internationally. The Cataract National Dataset Electronic Multi-centre Audit of 55,567 operations: anaesthetic techniques and complications. The Cataract National Dataset electronic multicentre audit of 55,567 operations: antiplatelet and anticoagulant medications. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Quality of life after first and second-eye cataract surgery: five year data collected by the Swedish National Cataract Register. Effect and outcomes of posterior capsule rupture in a district general hospital setting. Short-term outcomes in eyes with posterior capsule rupture during cataract surgery. Phacoemulsification cataract surgery and unplanned anterior vitrectomy-is it bad news? Evaluation of costs for cystoid macular edema among patients after cataract surgery. Acute endophthalmitis following cataract surgery: a systematic review of the literature. Pseudophakic retinal detachment after phacoemulsification cataract surgery: Ten-year retrospective review. Risk factors for retinal detachment after cataract surgery: a case control study. Retinal detachment after phacoemulsification in high myopia: analysis of 2356 cases. The Royal College of Ophthalmologists has a microsurgical skills faculty, which delivers courses in microsurgical skills over a three day course. Exemption for experienced surgeons from abroad can be sought from the chairman of the Surgical Skills Faculty who with the supervising consultant ensures certain basic skills have been achieved. Courses for higher surgical trainees covering the seven sub-specialty areas have been introduced including intermediate and advanced cataract surgery courses. Shortening the total training time All these factors have increased demands on the service and highlighted the importance of training in order to prevent the exposure of patients to any additional risk. Surgeons should be fully cognisant of the surgical techniques and the phaco-dynamics of the machine. Various practice eyes are available and it is recommended that beginners should attend one of the many courses held nationally. The Royal College of Ophthalmologists runs regular courses on basic phacoemulsification in its skills centre. Time taken to learn how to use the phacoemulsifier in the wet lab will 1 be repaid by faster and safer progress in the operating theatre. Live surgery should not be attempted until the surgeon is completely familiar with the machinery. Instruction and supervision by an experienced phaco-surgeon is essential and invaluable when transferring these skills to the operating theatre. In the early stages the component steps of the operation may be learnt separately before the surgeon completes the whole procedure. It is likely that in the future most hospitals will demand evidence of such structured training for any new surgical technique especially involving new apparatus. This should be seen as part of post-graduate development and evidence of such training or re-training kept in a personal revalidation folder. One such simulator is available at the College and is used in the basic microsurgical skills course. It is also available to book for trainers and trainees to use on a more ad hoc basis. Ideally, each training region would have a simulator as well as a more traditional skills centre to allow the development of regional training modules and facilitate practise. This can be in the form of a verbal agreement about what is expected, what the trainee should undertake, when the trainer will take over and how much time is allowed for training in a particular circumstance. This may be at the beginning of the list, or after a specified number of cases and everyone should be in agreement that the consultant or supervisor of the list will take over after the set time so that the list finishes on time; all the cases are done but everybody gets adequate exposure to surgery. It is the regular and frequent exposure to supervised training that will increase surgical speed, competence and confidence more than anything. Attendance at these courses facilitates the acquisition of teaching skills and learning theory. Ideally electronic systems should be available to allow the routine collection of data. Analysis of this data allows risk stratification of cases by complexity and by 2 seniority of surgeon. Outlining what the trainee can expect before the surgery starts is a good way of relieving the pressure on the trainer whilst the list is proceeding and, with the additional use of a wet lab out of the theatre environment, training time should be shortened considerably. Skills acquisition and assessment after a microsurgical skills course for ophthalmology residents. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Patient Safety and Clinical Risk in Cataract Surgery Quality and safety of patient care are intimately intertwined with clinical and organisational structures, clinical governance and good clinical management. Good planning and then doing the correct thing for the correct patient in the correct setting as well as learning from those occasions when incorrect care has occurred is a pragmatic lens through which to view these complex interrelated concepts. Quality and safety are intuitively recognised when present and glaringly obvious when absent. Patient safety and quality of care thus constitute the foundations of care and of service provision. Strict attention to detail, risk assessment and careful consideration of patient pathways is required for safe cataract care. However clinical errors, near misses, expected and unexpected surgical complications and events will happen. Such events may provide an opportunity for learning to reduce risk of similar events occurring again and occurring elsewhere. It is estimated that approximately 10% of healthcare episodes and interventions are compromised in some way by clinical error and 50% of which are preventable. It is thus argued that 10% of resources should be allocated to patient safety or quality matters. Investment in appropriate staffing levels, team training, appropriate equipment and development of a safety culture with patient involvement are key elements to modern safe cataract surgical care. A more enlightened view is that clinical risk management that focuses on patient safety will enhance the quality of care while reducing the health economic burden of patient harm. A patient safety incident can be defined as any unintended or unexpected incident which could have or did lead to harm for one or more patients. This is also referred to as an adverse event/incident or clinical error, and includes near misses. Medical errors may be regarded as adverse events or near misses that are preventable within the current state of medical knowledge. This should involve: risk assessment; the identification and management of patient-related risks; the reporting and analysis of incidents; and the capacity to learn from and follow-up on incidents and implement solutions to minimise the risk of them recurring. While there may be occasional poorly performing staff, most clinical errors are committed by well trained, well motivated individuals. Variability in surgical outcome has been attributed to the interplay of multiple factors including; surgical ability, surgical technique, case mix, case volume, institutional systems influences, peri-operative care and anaesthetic care. Improving safety of surgical care is a multi-faceted task and requires multi-disciplinary and organisational commitment and leadership. While all patient safety incidents result from clinical management, not all are preventable. For example, a patient having cataract surgery who suffers from postoperative endophthalmitis has had a serious patient safety incident. Root cause analysis of the case history, peri operative events, staffing issues, facilities, results of microbiology investigations etc, may clarify if it was a potentially preventable adverse incident (such as a sterilisation equipment failure or failure to use appropriate chemo-prophylaxis), or not. It can be helpful to consider patient safety issues by both underling causational risk factors and or subsequent consequence(s). Such as for new cataract surgical care commissioning plans and for new technology and devices and for off label use of medications. Insufficient continuous professional development of cataract surgeons and healthcare personnel. Inappropriate staffing levels with appropriate skills and lack of effective clinical leadership. Poor infrastructure and lack of investment in appropriate cataract surgical facilities and dedicated day care area. Failure of timely and appropriate management of surgical complications, including taking early second opinions and referral to tertiary centres. Last minute changes; such as late changes to operating lists or un-expected admissions. Both regular servicing and pre-operative checking of availability equipment required for cataract surgery is good practice. Consider the additional equipment that might be required for intra-operative complications or surgical surprises. Incidents due to incorrect use of Luer lock cannulae or failure to use Luer lock cannulae in cataract surgery continue to occur. This is particularly relevant to para-medical and nursing agency and bank staff and medical locums and use of visiting -including from overseas clinical teams to undertake additional surgical activity. Taking time out prior to commencement of surgery is recommended and as is a team brief at the start of the surgical session. This is especially relevant where dilutions for intraocular injection are prepared in the theatre such as when homemade dilutions of intracameral cefuroxime are prepared for intracameral injection. In relation to cataract care, post-operative endophthalmitis is the most feared outcome. Timely and evidence based treatment of both the individual patient with suspected endophthalmitis and the rigorous investigation of an outbreak are 4 needed. Advice from the College on the consideration of endophthalmitis clusters is available. Optimise biometry and customise A constants based on personal audits of refractive outcomes. Be aware of A constant differences with optical versus ultrasonic biometry measurements (See chapter on biometry). Swift access to resuscitation facilities and arrangements for rapid transfer to high dependency or intensive care facilities are precautions that should be considered in advance of potentially foreseeable problems and by both providers and commissioners of cataract care. Stand alone cataract treatment centers need to have robust pre-planned arrangements in this regard. Addition methods of learning from events, performance monitoring and systems improvements should also be deployed. Evidence of such endeavours might also form a part of the Appraisal and Revalidation of cataract surgeons and the accreditation of clinical services. Such serious adverse events from interventions that lead to significant harm or lasting disability, such as loss of sight, or are a cause for concern by staff, or patients, may be regarded as critical incidents. They may be preventable by a change of practice and are thus worthy of further investigation of root causes. Patient safety incidents in cataract care, regarded by the College as critical, are shown in Table 1. This list is intended to be a practical aid and is neither exhaustive nor exclusive. Such incidents in cataract care should be reported via incident reporting systems and should be reviewed at team meetings. Near misses have the potential to provide learning where patients have not been harmed. Table 1 Suggested critical patient safety incidents; cataract surgical care Operation on the wrong eye. Whether these patient safety incidents require further analysis is a matter for local organisations. It is best to arrange to see patient on first day following any significant intra operative complication. It can often be helpful to discuss clinical complications early with colleagues, including telephone consultations. Technical solutions to improved equipment and novel medications will come from clinical research. Senior doctors who shape a culture of clinical quality improvement and patient safety by personal example have a powerful and lasting effect on the members of their clinical teams and, via their training activity, on the next generation. Careful consideration of patient pathways including failure mode analysis and technology advances are of merit in risk reduction. Industries such as rail or air transport have shown that despite technical improvements and lessons learned there are still risks either apparent and unsolvable or latent. Adequate headroom and back up is a key precautionary principle of safe cataract surgery. Strict attention to detail, a focus on safety and learning from adverse events and near misses enhances cataract care. The College is committed to supporting steps that improve the safety of both cataract and ophthalmic care at both 1 individual and organisational levels.
To use the ophthalmoscope the practitioner sits or stands adjacent to the eye to be examined pain treatment with heat generic imdur 40mg with mastercard, preferably examining the right eye with his right eye and hand midsouth pain treatment center oxford ms generic 40 mg imdur free shipping, and the left eye with his left eye and hand midwest pain treatment center beloit wi purchase imdur us. If this is not seen treatment guidelines for back pain cheap imdur 20 mg line, then an opacity in the cornea pain treatment sickle cell cheap 40 mg imdur free shipping, a dense cataract or a vitreous opacity is indicated and fundal examination will not be possible pain treatment center in morehead ky buy imdur with american express. Once the red reflex has been seen, the practitioner moves the ophthalmoscope slowly towards the patient and at about 5 cm from the surface of the eye the retina and the optic disc should come into view. These can then be brought into focus by rotating the dial with the index finger until the most suitable lens is found. After examining the posterior pole the patient is asked to look directly into the ophthalmoscope light. It can be useful in refracting patients who are unable to participate in a subjective examination that requires judgement and response from the patient. By moving the light across the pupil the relative movement of the reflection or reflex can be observed. This is then neutralised by manually placing trial lenses in front of the eye until the most appropriate correction is found. The periphery of the fundus can be observed and the contrast of lesions such as naevi is improved. Indirect ophthalmoscopy can be carried out in two ways, by: G indirect slit lamp biomicroscopy and G use of an indirect ophthalmoscope. The patient sits at the slit lamp and the practitioner commonly uses a +90 or a +78 dioptre lens to 147 the ophthalmic study guide examine the fundus. The higher the dioptre of the lens, the lower the magnification, but the greater the field of view. However, the higher the dioptre is, the closer the lens needs to be held to the eye. This second method provides a good view of the peripheral retina and is commonly used to diagnose or to confirm diagnosis of retinal detachment, holes or tears. The practitioner places on his or her head an ophthalmoscope mounted on a headband (often referred to as an indirect). A 20+ dioptre lens is used for examining the fundus, giving a greater magnification and which can be held at a greater distance from the eye, thus providing a wider field of view. The practitioner must move his or her head and the lens in various directions to examine the different areas of the retina. As the image seen by the practitioner is inverted, the use of the indirect ophthalmoscope is a complex skill to master. During the examination the practitioner may use a scleral indenter (usually kept with the indirect). It has a small T-shaped probe that can be applied to the outside of the upper eyelid at the margin of the tarsal plate. When gentle pressure is exerted visualisation of the peripheral retina is further enhanced. The goniolens Gonioscopy is the examination and analysis of the angle between the posterior corneal surface and the anterior surface of the iris. It provides access to the trabecular meshwork through which aqueous outflow is controlled. Gonioscopy is, therefore, an important element in the examination of patients suspected of having glaucoma. The lens has one curved surface, which is applied directly to the cornea like a contact lens. Inside the lens is an arrangement of mirrors which may be a single, double or triple mirror. Mirrors enable the reflection of rays leaving the lens in an approximately perpendicular direction at the contact lens surface. The patient sits at the slit lamp and a local anaesthetic drop such as oxybuprocaine hydrochlo ride 0. The practitioner then lubricates the curved surface of the lens with a lubricant like Viscotears. The patient is asked to look straight ahead and his or her eyelids are held open and the lens tipped so that contact with the cornea is made at the 6 o?clock position, with the mirror at the 12 o?clock position. If a triple-mirror lens is being used, this will be the small domed 148 Ophthalmic equipment mirror. The lens is then rotated forward against the cornea and gently pressed against the eye to create a suction cup effect, which keeps it centred on the cornea. During examination the lens is rotated clockwise in order that the whole circumference can be viewed. As well as diagnosis and evaluation of the anterior chamber angle, the goniolens is used in laser procedures. In trabeculoplasty, for example, the use of a triple mirror enables simultaneous visual isation of a wider area of the angle. The B-scanner B-scan ultrasonography is a painless and non-invasive method of evaluating the eye in cases where the intraocular structures cannot be visualised. It is used for the diagnosis of retinal tears and detachments, particularly where there has been a recent vitreous haemorrhage. Ultrasound can be described as an acoustic wave that consists of an oscillation of particles within a medium. Ophthalmic B-scanning focuses a narrow acoustic beam across segments of the retina to produce a two-dimensional sector image. An echo is represented as a dot on the image and the strength of the echo is depicted by the brightness of the dot. The coalescence of multiple dots forms the two dimensional representation of the examined tissue section. Lubricating gel is applied to the scanning sensor, which is then passed over the eyelid. Fundal photography the fundus camera is a specialised, low-power biomicroscope with an attached camera that is used for photographing the retina. It is useful for providing a permanent record of the condition of the retina at a point in time, which can then be used for diagnosis and for future comparisons and evaluations. There is a chin rest and a headband, as on a slit lamp, to help position the patient. The camera is connected to a monitor so that the images can be assessed before printing. The optics of the fundus camera work on the principle that the illumination and observation light paths are separate. The observation light, or camera flash, reaches the eye through a series of lenses and a ring-shaped aperture. The reflected light from the retina passes back through the aperture system via two paths, one to the camera and one to the eyepiece. The fundal camera is used to monitor a number of conditions including glaucoma, diabetic retinopathy, age-related macular degeneration and vascular occlusions. Fundal photography is often used in conjunction with fluorescein angiography as a diagnostic procedure. In this procedure, an intravenous injection of fluorescein 20% (1g per 5 mL) is administered as the patient sits at the camera. As the fluorescein dye flows through the blood vessels of the eye a rapid series of photographs is taken. These record the flow through the choroidal and retinal blood vessels and can indicate areas of vascular leakage, neovascularisation or absence of flow through a vessel. Nurses administering the dye should be fully aware of the signs and symptoms of these reactions and be current in their 149 the ophthalmic study guide training to deal with them. The nurse should have an anaphylaxis box that contains the appropriate emergency drugs close at hand and they should know the exact whereabouts of the crash trolley. All patients experience skin discolouration and staining of their urine for about 24 hours following the procedure. A number of patients also experience skin flushing, sometimes accompanied by an itchy rash. More serious but rarely occurring adverse reactions include laryngeal oedema, bronchospasm and anaphylactic shock. This type of angiography is of particular value in studying the choroidal circulation. Adverse side effects are less common with this dye, however it does contain 5% iodine so should not be administered to patients with a known allergy. Less common are syncope, pyrexia, back ache, skin eruptions and localised skin necrosis. These symptoms should be outlined to the patient while gaining written consent for the procedure. A detailed history should also be taken, including any known allergies, cardiovascular conditions and details of previous diagnostic procedures using fluorescein or indocyanine green. Retinal imaging Specialist imaging devices are used increasingly in ophthalmic examinations and assessments. These also provide a record of the advance of disease, which can inform clinical management. Heidelberg retina tomograph this confocal scanning diode laser assesses the optic nerve head by creating a three-dimensional image. It is primarily used for the assessment and management of patients with glaucoma as it can measure the optic disc and the nerve fibre layer. In this system, a laser beam scans the fundus and the amount of light reflected from each scanned point is measured. It uses a low light intensity and images can be obtained through an undilated pupil. Optical coherence tomograph this is designed to provide high-resolution cross-sectional images of the retina. It operates on the same principle as ultrasound but uses an infrared light beam rather than acoustic waves. The image produced is a map of the intensity of the light reflected from the tissue structures of the retina. Different layers of the retina can be viewed because different tissue structures reflect the light with different intensities. The method is useful for diagnosing and monitoring a range of ophthalmic conditions including age related macular degeneration, central serous retinopathy, choroidal neovascularisation, macular oedema, glaucoma and optic nerve disorders. Even though it is still an emerging technique, it has the potential to reduce the need for more invasive assessments such as fluorescein angiography. It assesses the degree of any field loss 150 Ophthalmic equipment and is most frequently used in the monitoring of glaucoma. Other disease such as retinochoroidal lesions, optic nerve disease and neurological pathology will also produce characteristic patterns of field loss, which can be assessed with perimetry. The Humphrey field analyzer is an automated perimeter with an in-built computer that enables it to produce detailed and accurate results. The computer stores an age-match set of normal values so that results are presented as a comparison with normal values. The Humphrey field analyzer provides an objective assessment because it contains no bias from an examiner. First the patient details, including name, date of birth and hospital identification number are entered into the computer. The patient sits close to the field machine, which is then adjusted to the most comfortable height. The chin rests on an adjustable rest and the forehead is placed against a band, to help maintain the correct Fig. It should be explained to the patient that they need to fix their gaze on the central yellow light, which they will see on the field. The patient is given a handset and instructed to press a button every time they see one of these lights. They should be reassured that they can blink, and that each point of light is shown more than once. As the nurse supervises the test, the position of the gaze can be checked on the monitor. Ideally, the test should be carried out using near-vision correction and there is provision on the analyser for the placement of the appropriate lens in front of the eye. Find out how to check the reliability parameters on the Humphrey visual field test printout. The patient sits close to and in front of a field on which light stimuli are shown at predefined locations. The test determines the severity of field loss in terms of its size, shape and depth. The predefined pattern of stimuli presented to the patient is termed an algorithm and several different algorithms can be presented by the Humphrey field analyzer. This test reduces the test time without compromising its ability to detect glaucomatous field loss. The 24-2 test evaluates the temporal 24 degree and the nasal 30 degree areas of the visual field. Other algorithms which you may see used are the 76, the Central 30-2 (which evaluates points up to 30 degrees away from the centre of fixation) and the Estermann binocular field. They are written as a number between 1 and 40, which represent sensitivity to the stimulus. Test reliability can be affected adversely by several factors and it is the responsibility of the person supervising the test to minimise them.
The key objective for the dental care provider is to adopt a position that allows him or her to achieve optimal access pain treatment gout cheap imdur on line, visibility pain treatment center baton rouge louisiana order imdur 40 mg visa, comfort and control at all times treatment pain right hand order imdur on line amex. Ideally pain in thigh treatment order imdur 20mg amex, when providing patient care pain treatment center of illinois new lenox order imdur uk, muscles should be in a relaxed and well-balanced position with the exception pain treatment of herpes zoster order imdur 40 mg free shipping, of course, of those muscles performing the actual task. This is followed by a forward curve at the lower spine, a backward curve at the upper spine and ends with a forward curve at the neck. These curves allow the entire trunk to remain balanced over the center of gravity. Since the operator is most commonly in a seated position while working, the design and use of the 6 stool becomes a critical part of the balance. Variations in footwear such as high-heeled shoes or thick soles could demand a higher seating base. The operator should sit back as far as possible to take maximum advantage of 3 the lumbar support. If the operator uses a chair with arm rests, the arm rests should be fully adjustable to allow an operator full access to the patient while keeping elbows at their side. Many times the assistant is struggling with blocked vision and the only way to see is to lean forward. Without the belly bar to lean on, the assistant would probably come out of their seat. With the increased visibility the assistant could simply pivot the belly 3 rest around to the back of the chair and use it as a lumbar support. When seated, the assistant generally should maintain neutral posture with feet flat on the foot rest. At times it may be necessary to work in a standing position for a short period of time. A change in position, or periodic stretching provides necessary muscle relaxation to promote 4 good posture. Good posture promotes more energy, less stress and strain, less distraction from pain, and less errors. Bad posture results in pain, fatigue, poor work quality, negative 5 attitudes, and aging. Supine positioning of the patient in the chair is usually the most effective way to help maintain neutral posture. One result is that the maxillary occlusal plane of the patient is then perpendicular to the floor, creating the greatest access and the most effective visual line to the oral cavity. For most intraoral access sites, the maxillary plane should be extended 7 degrees beyond the vertical. For treating the maxillary second and third molars, the maxillary plane should be 25 degrees beyond the vertical. For the mandibular anterior teeth, bring the patients chin down so the 6 maxillary plane is 8 degrees ahead of the vertical. When gripping a small diameter handle (1/4 inch or less) the operator often grips the instrument with the very tips of the fingers. During movements requiring force this manner of grasping concentrates most of the strain within a very small set of hand muscles. Larger diameter instrument handles allow the operator to grip the instruments with the pads of the fingers and 2 consequently distribute the strain through a larger group of muscles. Because of this, manufacturers are developing a greater variety of handle sizes, shapes materials and textures which reduce the pinching effect and distribute forces over the pads 8 of the fingers. It is helpful to introduce variation, and balance of activities and instruments to shift the work to different muscle groups. For example, even the subtle variation between instruments of various handle size can distribute muscles activity among hand and finger 9 muscle groups, reducing fatigue. A round handle, as opposed to a hexagonal handle, with hard edges will reduce muscular stress and digital nerve compression. However, a smooth, round handled instrument requires more pinching force to keep the handle from spinning in the hand. Handles with shallow, circumferential grooves or with knurling (texturing) allow better friction with the fingers so that a secure grasp requires less force. Small diameter, hexagonal shaped instrument handles produce a mechanical stress that may cause digital nerve compression. Resistance from retractable or coiled hoses on dental units could result in extra mechanical 10 stress to maintain a precision grip. Unbalanced instruments, such as slow speed motors, feel heavier at one end causing the operator to compensate in their grip by increasing the mechanical stress to the fingers and hand. When instruments are wet and slippery or handles have smooth round surfaces force is increased to maintain a secure grip on the instrument. When the hand and wrist are moved out of neutral posture into a deviated or 10 awkward posture, the effort exerted should increase to accomplish the same work. When working edges are sharp, the instrument performs more of the work; when the edges are dulled, additional 10 operator force is required to achieve the same result. Practitioners should consider use of automatic instruments instead of manual hand instruments. The tension in the hose is transferred to the wrist and arm as the hose is stretched. Ideally, use a pliable hose with a swivel mechanism in the barrel of the hand-piece so that it can rotate 11 with minimal effort. Side delivery delivers at 8-9:00 But over the past two decades, there have evolved a large number of delivery systems primarily in the United States with units that deliver from the 2:00 position. Unlike rear delivery, the hand-pieces are accessible by both the operator and the assistant. When working in four handed dentistry the dentist maintains a position around the operating field with limited hand, arm and body movement, and should best confine eye focus to the working field. Additionally, the dental equipment and instruments should be centered around the dental assistant. From an ergonomic viewpoint, over-the-head and over-the-patient delivery systems better allow the dental assistant to access the hand-pieces for bur changes or other operations. When properly selected and adjusted, lighting and surgical magnification can support balanced musculoskeletal ergonomics. Conversely, of course, improperly selected or poorly adjusted systems can contribute to , or may even create, 13 unacceptable working postures. In general, the intensity ratio between task lighting (the dental operating light) and ambient room lighting should be no greater than 3 6 to 1. Once the patient and operator are properly positioned, the light source can be left far above the heads of both the operator and assistant because the correct position will require no adjustment during the procedure. It is important for the operator to keep his or her eyes on the oral cavity as much as possible and within the bright spot. Vision will stay sharp if the iris is not continually exercised by looking from the bright spot to dark places. With four-handed dentistry, instruments are delivered to the operator without need for them to move their eyes from the field of vision. To minimize eyestrain, the light from the fiber-optic hand-piece should be only slightly greater in intensity than that of the overhead task light, but not greatly so. It is important to make certain that the surgical magnification system fits the specific balanced neutral position of the operator using it. Maintaining a properly established working distance helps prevent the operator from assuming an awkward posture. With the requirement of keeping proper positioning using magnification the operator stays focused and relies on the assistant to anticipate and facilitate each step in the procedure. Considerations are magnification power, depth of field, declination angle, weight and convergence. Although the influence of gloves on hand discomfort has yet to be explored, they have been cited indirectly as a potential contributor 14-16 to carpel tunnel syndrome. Through self-reported surveys and anecdotal accounts, some operators attribute pain and discomfort at the base of the thumb to prolonged wearing of gloves. Dental assistants create a more efficient environment for the operator by eliminating unnecessary motion; decreasing twisting and turning movement; decreasing long reaches and unbalanced posture. Four-handed dentistry not only can increase productivity and efficiency it also might decrease stress and strain from awkward posture, twisting and turning, and frequent movement away from the operating field. Because dental work has become more sedentary, larger muscle groups, responsible for cardio-respiratory health and overall endurance, are relatively inactive. Extreme metabolic and functional demands are placed on the smaller muscle groups of the arms and hands. It is important to balance the sedentary with activities that promote conditioning and physical fitness. Injury could incur or a previous injury might be exacerbated by improperly performed exercises. Proper temperatures: Within the work environment, low room temperatures, manipulation of cold materials or instruments and exposure to cold air exhaust can contribute to low finger temperatures. There are no standards for finger temperatures, but it is recommended that hands and fingers be kept above 25 C or 77 F to avoid detrimental effects on 19 dexterity and grip strength. Alternate easy with difficult cases throughout the day and provide buffer periods that accommodate emergency patients or extra time for difficult procedures or patients. With difficult patients and procedures, alter the sequence of the tasks to be performed, whenever possible. For example, in order to increase task rotation, instead of scaling the entire mouth, then polishing all the teeth followed by flossing, consider doing these tasks a quadrant at a time. However, dentists should still be encouraged to implement task rotation throughout the day to whatever extent is possible. Ergonomic principles also extend to the staff involved in the administrative, non-clinical areas of the dental office. Clerical office workers have been widely studied, so 18 there are well-established ergonomic principles that can be followed. For example, the business office staff should use a chair with a seat that is comfortable and capable of supporting a balanced posture, and yet permits occasional variation in the sitting position. The chair height should be adjusted so that the thighs are horizontal to the feet flat on the floor. If using a keyboard, the chair should be adjusted such that the keyboard and a footrest keep the thighs parallel to the floor. The wrist/palm rest is not to be used while actually keying but in periods of rest. The forearm should be horizontal and at right angles to the upper arm, keeping elbows close to the side. A keyboard shelf under the counter or workstation places the keyboard at the correct height. The top of the computer screen should be at eye level with the top line of print slightly lower. The screen and document holder should be at the same distance from the eye yet close together enough so that the operator can look from one to the other without excessive movement of the neck and back. A screen that swivels horizontally and tilts vertically enables the operator to select the optimal viewing angle. Position the screen to minimize glare or use an anti-glare filter on the front of the screen. The workstation desk or counter should suit the kind of task being performed and be large enough to accommodate the other essential office supplies. It should provide for sufficient legroom to accommodate a comfortable seated position and the ability to swing from one work area to another without physical barriers or obstructions. It should be clear that not all of the interventions discussed above apply to all ergonomic situations. When to Take Action to Reduce Risk: Work-Related Musculoskeletal Disorders (lecture). Carpel Tunnel Syndrome Risk Factors and Preventive Strategies for the Dental Hygienist. The Ergo Factor: the Most Common Equipment and Design Flaws and How to Avoid Them. Evaluating the Fit of Ambidextrous and Fitted Gloves: Implications for Hand Discomfort. Some of these articles and studies have been cited in this paper; others have not. Inclusion of any article or study into this paper does not indicate endorsement of the methods or conclusions discussed in the articles. As noted in the disclaimer to the paper, significant shortcomings exist in the literature in this field. An Investigation of Ergonomic Interventions in Dental Hygiene Work Applied Ergonomics vol. Carpel Tunnel Syndrome Risk Factors and Preventive Strategies for the Dental Hygienist. The University of Michigan College of Engineering, Ann Arbor, Online Training, Inc. Elements of Ergonomics Programs: A Primer Based on Workplace Evaluations of Musculoskeletal Disorders. Health care and indemnity costs across the natural history of disability in occupational low back pain. A controlled prospective study with special reference to therapy and confounding factors. Low back disability among self-employed dentist, veterinarians, physicians and physical therapists in the Netherlands.
Generic imdur 20 mg fast delivery. Pcod!how to cure pcod polycystic ovarian disease by homeopathic medicine??.
Any underlying congenital or structural defect (blebs pain treatment and wellness center buy discount imdur online, bullae jaw pain treatment home purchase discount imdur on line, and so on) are disqualifying regardless of pneumothorax history pain treatment center richmond ky purchase imdur 20 mg without prescription. Clinical evaluation should include the following: (a) Normal pulmonary function testing allied pain treatment center oh imdur 20 mg low cost. Designated divers who experience a pul monary barotrauma following a dive with no procedural violations or a second episode of pulmonary barotrauma heel pain treatment yahoo order generic imdur on-line, are considered disqualified for diving duty pain treatment without drugs trusted 20mg imdur. A waiver request will be considered if the diver is asymptomatic after 30 days and must include: 1. Severe colitis, peptic ulcer disease, pancreatitis, and chronic diarrhea do not meet the standard unless asymptomatic on an unrestricted diet for 24 months with no radiographic or endoscopic evidence of active disease or severe scarring or deformity. Gastro esophageal reflux disease that does not interfere with or is not aggravated by diving duty is not considered physically disqualifying. Return to diving duty prior to 6 months post spontaneous vaginal delivery or caesarian section requires waiver request. In addition to current accession standards, any condition that compromises the performance and safety of the diver is disqualifying. Any condition that is exacerbated by continued diving service is also disqualifying. In addition to current accession standards, any condition that compromises the per formance and safety of the diver is disqualifying. Any condition that is exacerbated by continued diving service is also considered disqualifying. If a hyperbaric chamber is available, examinees will be tested for the inability to equalize pressure. Each candidate will be subjected, in a hyperbaric compression chamber, to a pressure of 60 feet sea water (41. This test should not be performed in the presence of a respiratory infection that may temporarily impair the ability to equalize or ventilate. The diver is free of any disease or condition that would endanger themselves, their dive team members, or compro mise successful completion of the mission. The diver is free of any acute or chronic disease or condition that will be exacerbated by continuation of diving duty and pose undue risk on the health and wellbeing of the diver. Distance visual acuity must be correctable to at least 20/20 in one eye and 20/40 in the other eye. Individual must pass one of the currently used color vision tests, without the use of color sensing lenses. Some Soldiers with certain medical conditions require administrative consideration when assignment to combat areas or certain geographical areas is contemplated. Such consideration of their medical conditions ensures these Soldiers are used within their functional capabilities without undue hazard to their health and well-being as well as ensures they do not produce a hazard to the health or well-being of other Soldiers. For example, a single acute adjustment disorder that resolved with a period of stability of over a year would pose no limitations pending combatant command guidance. While such individ uals may be completely asymptomatic at the time of examination, hypoxia due to residence at high altitude may aggravate the condition and result in further progression of the disease. Examples of areas where altitude is an important consideration are La Paz, Bolivia; Quito, Ecuador; Bogota, Colombia; and Addis Ababa, Ethiopia. Department of Veterans Affairs Disability Rating for Members of the Ready Reserve (Cited on title page. Function the function covered by this evaluation is service treatment records and healthcare documentation. Purpose the purpose of this evaluation is to assist medical, administrative, and recruiting command personnel in evaluating the key management controls listed below. Instructions these key internal controls must be formally evaluated at least annually or whenever the commander and/or designating authority changes. Answers must be based on the actual testing of key management controls (for example, document analysis, direct observation, sampling, other). Answers that indicate deficiencies must be explained and corrective action indicated in supporting documentation. Comments Help make this a better tool for evaluating the standards of medical fitness. To con stitute accepted medical principles, the deduction must be based upon the observation of a large number of cases over a significant period of time and be so reasonable and logical as to create a moral certainty that they are correct. Includes full-time training duty, annual training duty, and attendance, while in the active military service, at a school designated as a service school by law or by the Secretary of the military department concerned. Army National Guard That part of the organized militia of the several States and Territories, Puerto Rico, and the District of Columbia, active and inactive, that is a land force; is trained, and has its officers appointed, under the sixteenth clause of section 8, article I, of the Constitution; is organized, armed, and equipped wholly or partly at Federal expense; and is federally recognized. Enlistment the voluntary enrollment for a specific term of service in one of the Armed Forces as contrasted with induction under the Military Selective Service Act. Impairment of function Any anatomic or functional loss, lessening, or weakening of the capacity of the body, or any of its parts, to perform that which is considered by accepted medical principles to be the normal activity in the body economy. Latent impairment Impairment of function that is not accompanied by signs and/or symptoms but is of such a nature that there is reasonable and moral certainty, according to accepted medical principles, that signs and/or symptoms will appear within a reasonable period of time or upon change of environment. Manifest impairment Impairment of function that is accompanied by signs and/or symptoms. Medical capability General ability, fitness, or efficiency (to perform military duty) based on accepted medical principles. The presence of physical disability does not necessarily require a finding of unfitness for duty. The term physical disability includes mental diseases, other than such inherent defects as personality disorders, and primary mental deficiency. Physician A doctor of medicine or doctor of osteopathy legally qualified to prescribe and administer all drugs and to perform all surgical procedures. Regular Army A federal force of full-time Soldiers and Department of the Army civilians who make up the operational and institutional organizations engaged in the day-to-day missions of the Army. For purposes of this regulation, this includes both temporary and permanent disability retirement. Drugs that alkalinize urine (sodium bicarbonate, acetazolamide)pexcre tion,qeffects. Advise patient and parents to read the Medication death or ventricular arrhythmia), physical exam to assess for cardiac GuidepriortostartingtherapyandwitheachRxre? Abrupt cessation of high doses If exertional chest pain, unexplained syncope, or other cardiac symp maycauseextremefatigueandmentaldepression. Inform patient that the effects of drug-induced dry mouth can be minimized by odsandobservepatientforrebounddepressionaftertheeffectsofthemedication rinsingfrequentlywithwaterorchewingsugarlessgumorcandies. Instruct pa Disturbedthoughtprocess(SideEffects) tients to notify health care professional of any new numbness; pain; skin color 2015 F. Clarifcation of the required imaging for non-aneurysmal sub-arachnoid haemorrhage. Correction of previous error regarding the standard for untreated aneurysmal sub-arachnoid haemorrhage. Malignant intracranial tumours of childhood guidance now covers both infratentorial and supratentorial location. Clarifcation of the standard regarding Pulmonary Hypertension an established diagnosis. Chapter 4: Psychiatric disorders: Clarifcation with regard to the requirement of insight in relation to psychoses, mania/hypomania and schizophrenia/schizoaffective disorder. Clarifcation of the standards with regard to Neurological Developmental Conditions. Chapter 5: Alcohol and Drugs: No change Chapter 6: Visual disorders: Confrmation of the requirement for an uninterrupted horizontal feld of vision for Group 2 applications. Chapter 7: Renal and respiratory disorders: No change Chapter 8: Miscellaneous conditions: No change Appendices: Appendix B: Epilepsy regulations and further guidance Clarifcation with regard to provoked seizures, including confrmation that eclamptic seizures do not require time from driving. Information about the environment is via the visual and auditory senses and is acted on by many cognitive processes (including short-and long-term memory, and judgement) to effect decisions for the driving task in hand. These decisions are enacted by the musculoskeletal system, which acts on the controls of the vehicle and its relation to the road and other users. The whole process is coordinated by complex interactions involving behaviour, strategic and tactical abilities, and personality. In the face of illness or disability, adaptive strategies are important for maintaining safe driving. Safe driving requires, among other elements, the involvement of: vision visuospatial perception hearing attention and concentration memory insight and understanding judgement adaptive strategies good reaction time planning and organisation ability to self-monitor sensation muscle power and control coordination. Given these requirements, it follows that many body systems need to be functional for safe driving and injury or disease may affect any one or more of these abilities. The medical standards are continually reviewed and updated when indicated in light of recent developments in medicine generally, and traffc medicine in particular. In most cases, the medical standards for Group 2 drivers are substantially higher than for Group 1 drivers. This is because of the size and weight of the vehicle and the length of time an occupational driver typically spends at the wheel. Drivers who were awarded a Group 1 category B (motor car) licence before 1st January 1997 have additional entitlement to categories C1 (medium-sized lorries, 3. Drivers with this entitlement retain it only until their licence expires or it is revoked for medical reasons. On subsequent renewal or reapplication, the higher medical standards applicable to Group 2 will apply. Under certain circumstances, volunteer drivers may drive a minibus of up to 16 seats without category D1 entitlement. Age limits for licensing Group 1 Licences are normally valid until 70 years of age (the til 70 licence) unless restricted to a shorter duration for medical reasons. There is no upper age limit to licensing, but after 70 renewal is required every 3 years. A person in receipt of the mobility component of Personal Independence Payment can hold a driving licence from 16 years of age. Group 2 licences must be renewed every 5 years or at age 45 whichever is the earlier until the age of 65 when they are renewed annually without an upper age limit. All initial Group 2 licence applications require a medical assessment by a registered medical practitioner (recorded on the D4 form). The same assessment is required again at 45 years of age and on any subsequent reapplication. Any responsibility for determining higher medical standards, over and above these licensing requirements, rests with the individual force, service or other relevant body. Taxi licensing Responsibility for determining any higher standards and medical requirements for taxi drivers, over and above the driver licensing requirements, rests with Transport for London in the Metropolitan area, or the Local Authority in all other areas. Any responsibility for determining higher medical standards, over and above these licensing requirements, rests with the individual force, service or other relevant body. Sudden disabling events Anyone with a medical condition likely to cause a sudden disabling event at the wheel, or who is unable to control their vehicle safely for any other reason, must not drive. These fgures, while originally defned by older studies, have since been revalidated by more recent risk-of-harm calculations. They should also adhere, with ongoing consideration of ftness to drive, to prescribed medical treatment, and to monitor and manage the condition and any adaptations. Of course, this last obligation on professionals may pose a challenge to issues of consent and the relationship between patient and healthcare professional. For people with licences issued by the Driver and Vehicle Agency in Northern Ireland, the options for direct notifcation are given on the In our guidance Confdentiality: good practice in handling patient information we say: 1. Trust is an essential part of the doctor-patient relationship and confidentiality is central to this. Patients may avoid seeking medical help, or may under-report symptoms, if they think that their personal information will be disclosed by doctors without consent, or without the chance to have some control over the timing or amount of information shared. Doctors owe a duty of confidentiality to their patients, but they also have a wider duty to protect and promote the health of patients and the public. If it is not practicable to seek consent, and in exceptional cases where a patient has refused consent, disclosing personal information may be justified in the public interest if failure to do so may expose others to a risk of death or serious harm. If you consider that failure to disclose the information would leave individuals or society exposed to a risk so serious that it outweighs patients and the public interest in maintaining confidentiality, you should disclose relevant information promptly to an appropriate person or authority. You should inform the patient before disclosing the information, if it is practicable and safe to do so, even if you intend to disclose without their consent. Doctors owe a duty of confdentiality to their patients, but they also have a wider duty to protect and promote the health of patients and the public. This means they need to know if a person holding a driving licence has a condition or is undergoing treatment that may now, or in the future, affect their safety as a driver. Doctors should therefore alert patients to conditions and treatments that might affect their ability to drive and remind them of their duty to tell the appropriate agency. If a patient has a condition or is undergoing treatment that could impair their ftness to drive, you should: a. If a patient refuses to accept the diagnosis, or the effect of the condition or treatment on their ability to drive, you can suggest that they seek a second opinion, and help arrange for them to do so. As long as the patient agrees, you may discuss your concerns with their relatives, friends or carers. If you become aware that a patient is continuing to drive when they may not be ft to do so, you should make every reasonable effort to persuade them to stop. If the patient objects to the disclosure, you should consider any reasons they give for objecting. The College of Optometrists offers similar guidance, available in full at its website under the confdentiality section of its Guidance for Professional Practice (use the subsection on disclosing information about adults without their consent). This guidance includes the following (reproduced with permission of the College of Optometrists): (C73) If you think the patient may be engaging in an activity where they pose a very real risk of danger to the public or themselves, such as the patient driving when they are not fit to drive, but you are not sure whether you should act, ask yourself: 1. Information on the medical condition is sought from the licence holder or applicant, either by paper questionnaire or online 2. Information is sought from relevant healthcare professionals, either by questionnaire or provision of medical notes.
References
- Smith DJ, Bouchal RL, deSantic CA, et al. Properties of the interaction between ketamine and opiate binding sites in vivo and in vitro. Neuropharmacology 1987;26:1253-1260.
- Hawkins RD, Hon GC, Ren B. Next-generation genomics: an integrative approach. Nat Rev Genet 2010;11:476-86.
- Zhang HG, Wang J, Yang X, et al. Regulation of apoptosis proteins in cancer cells by ubiquitin. Oncogene 2004;23(11):2009-2015.
- Jollis JG, Peterson ED, DeLong ER, et al. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med 1994;331:1625.
- Matsumae H, Yoshida Y, Ono K, et al: CCN1 knockdown suppresses neointimal hyperplasia in a rat artery balloon injury model, Arterioscler Thromb Vasc Biol 28(6):1077-1083, 2008.
- Latham R, Lancaster AD, Covington JF, et al. The association of diabetes and glucose control with surgical-site infections among cardiothoracic surgery patients. Infect Control Hosp Epidemiol. 2001;22:607-612.
- Shah AJ, Kilcline BA. Trauma in pregnancy. Emerg Med Clin North Am. 2003;21:615-629.
- Ross W. Alkylating agents. In: Ross W, ed. Biological Alkylating Agents. London: Butterworths; 1962.