T. Andrew Bowdle, MD, PhD
- Professor of Anesthesiology and Pharmaceutics
- Chief of the Division of Cardiothoracic Anesthesiology
- Department of Anesthesiology
- University of Washington
- Seattle, Washington
Partly from Bonney V treatment molluscum contagiosum purchase neurontin 300 mg overnight delivery, Gynaecological Surgery treatment guidelines generic neurontin 600mg overnight delivery, Baillere Tindall symptoms viral meningitis purchase genuine neurontin online, 2nd ed 1974 with kind permission sewage treatment cheap neurontin 800mg with mastercard. Remove the suture immediately if: (4) Local vaginal or possibly intra-uterine infection medicine vs medication purchase generic neurontin canada. Very occasionally implantation is in the abdominal cavity (2) You have explained precisely what you are going to do medicine 666 quality 100mg neurontin, (20. Trouble occurs either because the and that the suture must be removed at 37wks, tube ruptures, or because the gestation aborts through the or when labour starts. The periods are usually a few days to a few months late, and she may rightly think she is pregnant. Or, she may not think she is pregnant because: (1) the tube may rupture before she has missed a period. If the period of amenorrhoea is short, before the symptoms start, gestation is likely to be in the isthmus, and the effects of rupture worse. An acute rupture presents as a sudden severe lower abdominal pain, with signs of hypovolaemia. Peripheral shutdown, tachycardia and drop in blood pressure ensue as shock progresses. A, the fimbria (the most red or brown vaginal bleeding usually follows 24hrs after common abnormal site) B, the ampulla, C, the isthmus. D, the uterine the onset of the pain, as the decidua are shed if the bleeding part of the tube. A subacute rupture typically presents with a history of 3-7days of weakness, anaemia and abdominal swelling, the common sites (20-3A,B) are the distal fi of the tube. The lower abdomen may be tender, Here, the results may be: with rebound tenderness and guarding, but these signs are (1);an acute or subacute rupture 6-10wks after the last often minimal. Blood irritating the diaphragm may cause period, referred pain at the tip of the shoulder. The presentation may (2) a tubal miscarriage, in which the foetus is expelled into be with diarrhoea and vomiting in up to 40% of cases. Instead, chronic bleeding may continue slowly urgent; you should perhaps cross-match blood first. A chronic ectopic gestation presents as lower abdominal In the uterine part of the tube (20-3D), it ruptures early. Both close to the internal os (20-3G), the diagnosis is usually easy when there has been massive resulting in placenta praevia, and in the cervix (20-3H) bleeding in the abdominal cavity but it can be very difficult, it leads to antepartum vaginal haemorrhage. If an ectopic gestation survives to 20wks Remember that any woman with a menstrual irregularity without causing serious symptoms, it is probably in one of (a period or more missed or periods which have been lighter the less common sites, perhaps in an angle. Patients with an ectopic gestation form 5 groups: Anaemia, dizziness, shoulder pain, and a tender mass are all (1). Those who have had a massive bleed into the abdominal extras which encourage the diagnosis, but are not necessary cavity. The gestation attaches itself to an area in the abdomen or ultrasound, you may be better off performing a laparoscopy sometimes inside the broad ligament where there is enough or mini-laparotomy as an ectopic gestation is potentially room even to grow to term! Those presenting early because they think they are salpingitis or appendicitis in the absence of an pregnant, often symptomless, where an ultrasound finds the intra-uterine gestation, you will have correctly intervened uterus empty while there is a pregnancy seen elsewhere, even if for the wrong reasons! Look for general signs of blood loss loses blood fast without having an infusion of fluid will die, (shock and anaemia), and for signs of bleeding within the if she does so, not from lack of red blood cells but from lack abdomen. This is the basis of hypovolaemic tenderness and guarding are variable, and may be absent. If there is a large tender mass in the lower abdomen, If then she arrives in shock and is operated immediately and bleeding has been confined there by adhesions. The important signs However, if she has had volume replacement before arriving are pain on moving the cervix, tenderness in the posterior in hospital, or in hospital while waiting to be operated upon, fornix and pouch of Douglas, and perhaps acute adnexal or whilst bleeding over a prolonged period, then her tenderness, which is worse on one side (highly suggestive). With volume just gone home: you may make bleeding get worse or even replacement but continuous bleeding, the cause of death is re-start! A few days after a severe bleed, however, you may find an Also because the blood in her abdomen is now partly diluted Hb as low as 3g/dl. In case of <1-1fi5l (the younger she is, usually the stronger) she does doubt, run 200ml of normal saline via a giving set and not really need to be (auto) transfused unless she was cannula into the abdomen. If possible these patients (with infusions If clear fluid runs back in the system you can exclude a running) should be operated immediately and perhaps ruptured ectopic gestation. If the patient is stable at the end of the operation and has enough circulating volume and you are certain you have stopped the bleeding, then a blood transfusion is often not needed. Do not use thiopentone over the lung bases, an impossibility to lie horizontally, for induction: the blood pressure might crash! Check the Hb: if <5g/dl, transfuse the Hb being 6g/dl by now, the nurse there even more strongly refused to give anaesthesia. The patient was now transported to the provincial hospital 1 unit of red cells if available. Neither surgeon nor Remember transfusions are often just giving you an extra anaesthetist wanted to intervene, so she was now referred to a Central margin of safety. In those cases bleeding can be often stopped immediately Since one ectopic gestation is followed in 30% of cases by even without access to a fully equipped theatre. This fluid might actually kill the patient as a result of inducing cardiac failure. Stop any bleeding (suction curetting with 6mm Karman curette without anaesthesia or twisting off a pedunculated fibroid. As soon as you open the abdomen while the patient is in Do not be too enthusiastic to restore the blood pressure Trendelenburg position (otherwise the blood will spill over and is not available for auto-transfusion) lift out the uterus if possible, find the above 90mmHg systolic, because you might promote more ruptured Fallopian tube and if it is still bleeding significantly, grasp the bleeding. Your first priority is to stop the bleeding: mesosalpinx between your finger and thumb, so as to compress and resuscitation is to prepare the patient as best you can in the later clamp the vessels and stop the bleeding. There will be blood in to insert the needle of a blood letting system as used by the abdominal cavity, which should not spill out and be lost blood banks, through the abdominal wall into the pool of for auto-transfusion. Find the ruptured Fallopian tube, and if it is still actively bleeding, grasp its broad ligament between your finger and thumb, so as to compress the vessels in it (20-4). Apply long curved haemostats across the tubes on either side of the ectopic gestation (20-5) so that the points meet and you leave no part of the broad ligament unclamped. You can put the distal clamp either over the distal tube (20-5X) or over the remaining broad ligament (20-5Y) which will result in removal of the distal tube. If you leave the fimbria, it may prove possible later to reconstruct the tube, provided there is >4cm of it remaining, if the patient becomes infertile. On the other hand, it is possible that a zygote fertilized in the contralateral tube might be trapped in the distal part of the amputated tube, resulting in another ectopic gestation. Suck out and discard the last drops of blood, so you can see where to place ligatures at the right place. If the other tube seems severely damaged, record it and tell Remove the ruptured part of the tube by cutting along the the patient. Place 2 long-acting absorbable cannot become pregnant anymore, achieve pregnancy ligatures under the joints of each clamp. Place double ligatures on both If there is a subacute ectopic, the ruptured tube will be sides, to make sure that no arteries are missed. Tie these ligatures carefully, or else postoperative If the patient has no other children and the tube looks bleeding will ensue. If bleeding continues after you have applied 2 ligatures, it is on occasion (provided the patient has easy access to a re-apply the clamps and repeat the procedure. Remove the gestation bluntly, by combining squeezing and using the Often, however, it is most reasonable to excise the affected back of dissecting forceps, and then very thoroughly tube completely; if you do so, remove the fimbrial end compress the area to stop the bleeding. Lavage the peritoneal cavity thoroughly with the mesosalpinx around the blood vessels supplying the area. If the patient has previously consented, Repair the incision in the tube with 5/0 sutures. In the middle of an ill-defined closed distal end, and the patient is stable, it is occasionally placenta and blood clot you will see the amniotic sac. Treat the anaemia with folic acid remove it anyway if you have opened the abdomen: try not orally and/or iron or if the Hb is <5g/dl with blood to spread infection, and lavage the pelvis afterwards with transfusion. Make sure you have tipped the head of the table down If you damage it, perform an appendicectomy (14. Feel for the uterus in If there is no ectopic gestation, and you find copious the midline in the hollow of the sacrum. Very occasionally there is blood in the abdomen uterus, feel for the affected tube. Before you remove the ovary (if you have into the peritoneum, and may be quite large (12-16wk size to), make sure you separate adhesions between it and the or larger). The blood supply to the tube and ovary comes from: Try one of the following 3 methos: (1);The ovarian vessels in the infundibulopelvic ligament. This will open the top of the If there is a raw area in the peritoneum which oozes, broad ligament. As you approach the infundibulopelvic after you have removed the ectopic gestation, it will usually ligament, find, clamp and divide the ovarian vessels without stop spontaneously, if there are no obviously bleeding including the ureter! Now you can clamp and divide the to ooze, insert a drain for 24hrs, and monitor the patient tube and ovarian ligament. If oozing from the base of the broad If you find inflamed tubes with some pus discharging from ligament does not stop spontaneously, clamp and tie the their fimbriated ends, or evidence of inflammation without bleeding vessels. Cut a ficm opening in the back of the If there is a chronic pyosalpinx, excising it will be very broad ligament, and squeeze out the haematoma by pressing risky if it has stuck to the bowel, but this may be possible if it from below. If you find no specific bleeding point, but only a general ooze, compress the area with a pack, and wait 10mins by the clock. If a pack fails to control the bleeding, tie or underrun as many bleeding vessels as you can. If you find clear fluid, this might be from a gestational sac in the pouch of Douglas. You will be able to aspirate blood if the haematocoele is in the pouch of Douglas, but not if it is, rarely, elsewhere. When there is extra-uterine implantation, inadequate attachment usually causes sudden bleeding. She had missed two periods and said that she had (1) One which has, so far, only caused a small bleed, with passed clots. She was anaemic, the uterus was slightly enlarged, and the cervix was closed and still bleeding. There were (2);One in which repeated small bleeds have caused a few curettings, so he thought that she must have had a complete haematoma (pelvic haematocoele, 20-7) containing miscarriage. He prescribed iron tablets and discharged her, but she 100-500ml of blood and clot. So she went to another hospital where the doctor felt a tender mass on the left side of the uterus. Moving the cervix is painful, feelings of fainting, and particularly if she has previously but this is not such a reliable sign as in an acute rupture. If it implants at the point where the tube enters the uterus, it ruptures early, but if it implants in the intramural part of the tube near the uterine cavity (angular or cornual gestation), it may not rupture until 20wks (20-3). If, rarely, an ectopic gestation implants in the cervix (cervical gestation), the cervical os will be open and contain a thin-walled cavity in which you can feel fragments of chorionic tissue. This cavity bleeds massively, and may resemble a miscarriage, where the cervical os is closed tight. Whereas there is little bleeding after a miscarriage has been evacuated, a cervical ectopic gestation continues to bleed profusely (20. Perform a laparotomy; you will find a purple bleeding mass arising from one angle of the uterus. The uterine and ovarian arteries supply this area, so irritation (with grimacing on coughing) bleeding can be very severe and many patients with this diagnosis will die before they reach hospital. Suggesting a threatened, incomplete, or complete miscarriage: significant vaginal bleeding. You can make a Remove all products of conception bluntly with your finger decidual cast disintegrate between your fingers, and then suture the open area with large bites of unlike placenta/trophoblast which will have villi clearly #2 long-acting absorbable suture. Be careful that you do not remove Suggesting a fibroid uterus in pregnancy: a solid mass too much of the outer layer of the uterus: otherwise there with much less discomfort. If there are many dense adhesions between the ectopic gestation and the surrounding organs, scoop out as much Pack the thin-walled cavity in the cervix tightly to stop blood clot as will easily come out without tearing and bleeding, and resuscitate the patient. If you injure the rectum or sigmoid colon, suture the If a pack does not control bleeding, there are 3 more injury and wash the pelvis thoroughly with warm water. Provided you do not go above this gestation), which is quite separate from it, and which you level the ureters will be safe. A distended abdomen which is like a full term gestation, (but perhaps kink) the ureter. Then insert a large (50ml or more) Foley catheter into the On questioning, the patient may later admit having missed bleeding cavity in the cervix, inflate the balloon, and leave it some periods, possibly several, in the past. Be careful not to penetrate the bladder as sometimes it the history is seldom helpful, but: needs to be dissected down. If this too fails, perform a (1) she may have had episodes of pain in early pregnancy; hysterectomy (21.
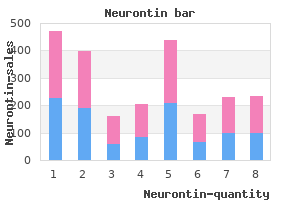
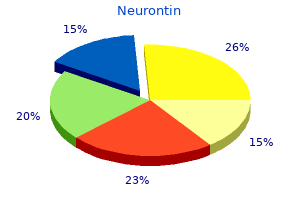
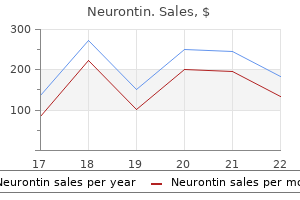
Dipyridamole-thallium testing is preferred for patients with known cardiac arrhythmias symptoms 0f yeast infectiion in women order genuine neurontin, and dobutamine is preferred for patients with bronchospastic lung disease and in those with severe cardiac stenosis (188) medicine pill identification quality neurontin 400mg. Coronary angiography should be considered only in patients who have an indication for angiography independent of the planned surgery medicine zebra 800mg neurontin, such as patients with acute coronary syndromes medications 25 mg 50 mg purchase neurontin 800mg free shipping, unstable angina medicine man 1992 order cheapest neurontin and neurontin, angina refractory to medical therapy medicine knowledge neurontin 400 mg, or high-risk results on noninvasive testing. Controversy exists regarding the accuracy of these tests to provide prognostic information beyond what is obtained from clinical risk stratification for nonvascular procedures. Diagnostic testing should not lead to unnecessary additional testing or harmful delays in s urge ry. The American College of Cardiology and the American Heart Association present an updated detailed algorithm that incorporates risk-factor stratification to guide clinicians to proceed directly to surgery, to delay surgery and obtain preoperative noninvasive testing, or to attempt risk factor modification (179). It is rare for patients who are younger than 50 years and who do not have diabetes, hypertension, hypercholesterolemia, or coronary artery disease to suffer a perioperative myocardial infarction. In contrast, patients with coronary artery disease are at increased risk of myocardial infarction in the postoperative period. Prevention, early recognition, and treatment are important because myocardial infarctions that occur in the postoperative period have mortality rates of up to 25% and are associated with increased rates of cardiovascular death in the 6 months following surgery (189). Nearly two-thirds of postoperative myocardial infarctions occur during the first 3 days postoperatively (189). Although the pathophysiologic factors are complex, the causes of postoperative myocardial ischemia and infarction are related to decreased myocardial oxygen supply coupled with increased myocardial oxygen requirements. In postoperative patients, conditions that decrease oxygen supply to the myocardium include tachycardia, increased preload, hypotension, anemia, and hypoxia (190). Conditions that increase myocardial oxygen consumption are tachycardia, increased preload, increased afterload, and increased contractility. Tachycardia and increased preload are the most important causes of ischemia, because both conditions decrease oxygen supply to the myocardium while simultaneously increasing myocardial oxygen demand. Tachycardia decreases the diastolic time, which, when the coronary arteries are perfused, decreases the volume of oxygen available to the myocardium. Increased preload increases the pressure exerted by the myocardial wall on the arterioles within it, thus decreasing myocardial blood flow. Other factors associated with perioperative myocardial ischemia include physiologic responses to the stress of intubation, intravenous or arterial line placement, emergence from anesthesia, pain, and anxiety. These stresses result in catecholamine stimulation of the cardiovascular system, resulting in increased heart rate, blood pressure, and contractility, which may induce or worsen myocardial ischemia. Loss of intravascular volume because of third spacing of fluids or postoperative hemorrhage can induce ischemia. Chest pain, which is present in 90% of nonsurgical patients with myocardial infarction, may be present in only 50% of patients with postoperative infarction because myocardial pain may be masked by coexisting surgical pain and the use of analgesics (175). It is important to maintain a high level of suspicion for postoperative infarction in patients with coronary artery disease. The presence of arrhythmia, congestive heart failure, hypotension, dyspnea, or elevations of pulmonary artery pressure may indicate infarction and should prompt a thorough cardiac investigation and electrocardiographic monitoring. Many patients will exhibit P-wave changes that spontaneously resolve and do not represent ischemia or infarction. In a review of over 2,400 patients, the sensitivity of predicting postoperative cardiac events was 55% to 100%, specificity 37% to 85%, positive predictive value 7% to 57%, and negative predictive value 89% to 100% (192). Postoperative management of patients with coronary artery disease is based on maximizing delivery of oxygen to the myocardium and decreasing myocardial oxygen utilization. Anemia is detrimental because of loss of oxygen-carrying capacity and resultant tachycardia and should, therefore, be carefully corrected in high-risk patients. Although transfusion criteria are not absolute, all patients with a hemoglobin less than 6 mg/dL, and hemoglobin of 6 to 10 mg/dL with significant cardiac risk factors should be offered blood transfusion (193). Patients with coronary artery disease may benefit from pharmacologic control of hyperadrenergic states that result from increased postoperative catecholamine production. Beta-blockers decrease heart rate, myocardial contractility, and systemic blood pressure, all of which are increased by adrenergic stimulation. Consider initiating and titrating beta-blockers in patients with coronary artery disease or high cardiac risk (as defined by the presence of more than one clinical risk factor) who are undergoing intermediate-risk surgery (155). Therapy should be initiated at least 1 week before surgery to allow for proper titration. The timing and optimal duration of beta-blocker therapy remains an area of uncertainty. Nevertheless, for patients already on beta-blocker therapy, they should continue it perioperatively because abrupt withdrawal results in a rebound hyperadrenergic state. Prophylactic use of other agents such as nitroglycerin and calcium-channel blockers remains controversial, as data did not show a consistent benefit toward reducing risk of ischemic cardiac events. The postoperative development of pulmonary edema may be associated with a high mortality rate, especially if it occurs in the setting of cardiac ischemia (198,199). Treatment usually relies on aggressive diuretic therapy, although care must be taken to avoid dehydration, which may result in hypotension during the induction of anesthesia. Hypokalemia can result from diuretic therapy and is especially deleterious to patients who are taking digitalis. In addition to diuretics and digitalis, treatment often includes the use of preload and afterload-reducing agents. It is preferable to continue the usual regimen of cardioactive drugs throughout the perioperative period. Other common postoperative causes are myocardial infarction, systemic infection, pulmonary embolism, and cardiac arrhythmias. The cause of postoperative heart failure must be diagnosed because, to be successful, treatment should be directed simultaneously to the underlying cause. Treatment of pulmonary edema may include the use of intravenous furosemide, supplemental o x yge n, morphine sulfate, and elevation of the head of the bed. Electrocardiography, in addition to laboratory evaluation, including arterial blood gas, serum electrolyte, and renal function chemistry measurements, should be obtained expediently. Arrhythmias Nearly all arrhythmias found in otherwise healthy patients are asymptomatic and of limited consequence. In patients with underlying cardiac disease, however, even brief episodes of arrhythmias may result in significant cardiac morbidity and mortality. Preoperative evaluation of arrhythmias by a cardiologist and anesthesiologist is important because many anesthetic agents and surgical stress contribute to the development or worsening of arrhythmias. In patients undergoing continuous electrocardiographic monitoring during surgery, a 60% incidence of arrhythmias, excluding sinus tachycardia, are reported (201). Patients with heart disease have an increased risk of arrhythmias, most commonly ventricular arrhythmias (201). Patients without cardiac disease are more likely to develop supraventricular arrhythmias during surgery. Patients taking antiarrhythmic medications before surgery should continue taking those drugs during the perioperative period. Initiation of antiarrhythmic medications is rarely indicated preoperatively, but consultation with a cardiologist is recommended for patients in whom arrhythmias are detected before surgery. Before performing surgery on patients with a permanent pacemaker, the type and location of the pacemaker should be determined because electrocautery units may interfere with demand-type pacemakers (203). When performing gynecologic surgery on patients with pacemakers, it is preferable to place the electrocautery unit ground plate on the leg to minimize interference by preventing the pacemaker generator from sitting within the electrocautery circuit and to maximize distance from the pacemaker device. If possible, use of bipolar cautery devices are recommended rather than monopolar devices. In patients with a demand pacemaker in place, the pacemaker should be converted preoperatively to the fixed-rate (or asynchronous) mode. Although this can be accomplished oftentimes by placing a magnet over the pacemaker, it may be better to reprogram the pacemaker preoperatively and then again postoperatively. Patients should be monitored continuously intraoperatively with both telemetry and continuous pulse oximeter. Patients with an implantable cardioverter defibrillator device should have their device programmed off prior to surgery and reprogrammed postoperatively (155). Surgery is not contraindicated in patients with bundle branch blocks or hemiblocks (204). Complete heart block rarely develops during noncardiac surgical procedures in patients with conduction system disease. The presence of a left bundle-branch block may indicate the presence of aortic stenosis, which can increase surgical mortality if it is severe. Patients with significant aortic stenosis appear to be at greatest risk, which is increased in the presence of atrial fibrillation, congestive heart failure, or coronary artery disease. Significant stenosis of aortic or mitral valves should be repaired before elective gynecologic surgery (176). The classic history presented by patients with severe aortic stenosis includes exercise dyspnea, angina, and syncope, whereas symptoms of mitral stenosis are paroxysmal and effort dyspnea, hemoptysis, and orthopnea. Severe stenosis of either valve is considered to be a valvular area of less than 1 cm, and diagnosis can2 be confirmed by echocardiography or cardiac catheterization. Electrocardiogram with high R waves, depressed T waves in lead I, and precordial leads Mitral stenosis 1. Electrocardiogram with large P waves and right axis deviation Patients with valvular abnormalities are subdivided by the American Heart Association into risk groups for the development of subacute bacterial endocarditis following surgery. Patients in the highest risk groups should receive prophylactic antibiotics immediately preoperatively to prevent subacute bacterial endocarditis (Table 22. As defined by the American Heart Association, only patients with prosthetic cardiac valves, congenital heart disease, and cardiac transplantation who develop cardiac valvulopathy should receive perioperative endocarditis prophylaxis (76). All other patients do not require antibiotics for subacute bacterial endocarditis prophylaxis. Patients with aortic and mitral stenosis tolerate sinus tachycardia and other tachyarrhythmias poorly. In patients with aortic stenosis, sufficient levels of digitalis should be provided to correct preoperative tachyarrhythmias, and propranolol may be used to control sinus tachycardia. Patients with mitral valve stenosis often have atrial fibrillation and, if present, digitalis should be used to reduce rapid ventricular response. If the patient is taking aspirin therapy, it should be discontinued 1 week before the procedure and restarted as soon as it is considered safe by the surgeon. Patients with a bileaflet aortic valve with no risk factors (atrial fibrillation, previous thromboembolism, left ventricular dysfunction, a hypercoagulable state, older generation thrombogenic valve) generally do not require anticoagulation bridging. Warfarin should be stopped 72 hours prior to the procedure and resumed 24 hours after the procedure. The heparin drip should be stopped approximately 6 to 8 hours before the procedure and restarted as soon as possible after surgery when the patient is deemed stable from postoperative bleeding risk. In the postoperative period, patients with mitral stenosis should be carefully monitored for pulmonary edema because they may not be able to compensate for the amount of intravenous fluid administered during surgery. Patients with mitral stenosis frequently have pulmonary hypertension and decreased airway compliance. They may require more pulmonary support and therapy postoperatively, including prolonged mechanical ventilation. For patients with significant aortic stenosis, it is imperative that a sinus rhythm be maintained during the postoperative period. Supraventricular dysrhythmias may be controlled with verapamil or direct-current cardioversion. Particular attention should be provided to the maintenance of proper fluid status, digoxin levels, electrolyte levels, and blood replacement. Hypertension Patients with controlled essential hypertension have no increased risk of perioperative cardiac morbidity or mortality (208). Patients with concomitant heart disease are at elevated risk and should be completely evaluated by a cardiologist preoperatively. Beta-blockers should be continued, parenterally if necessary, to avoid rebound tachycardia, hypercontractility, and hypertension. It may be prudent to withhold these agents on the morning of surgery and resume them postoperatively when good renal function and euvolumia is confirmed (155). Patients with diastolic pressures higher than 110 mm Hg or systolic pressures higher than 180 mm Hg should receive medication to control their hypertension before surgery. Beta-blockers may be particularly effective agents for treatment of preoperative hypertension (179). Chronically hypertensive patients are very susceptible to intraoperative hypotension because of impaired autoregulation of blood flow to the brain and require a higher mean arterial pressure to maintain adequate perfusion (209). During induction of anesthesia, episodes of hypertension occur, and such episodes are seen more frequently in patients with baseline hypertension. Postoperative hypertension is usually treated parenterally because gastrointestinal absorption may be diminished, and transdermal absorption can be erratic in patients who are cold and rewarming. With the evolution of bare metal and drug-eluting stents, perioperative management of cardiovascular thrombotic risk versus perioperative bleeding and mortality is challenged. Ultimately the risk of perioperative morbidity secondary to bleeding must be weighed against the risk of repeat thrombosis and cardiovascular morbidity and mortality. If a patient requires new placement of a cardiac stent and requires a noncardiac surgery in the following 12 months, placement of a bare metal stent is recommended rather than a drug-eluting stent, as these require only 4 to 6 weeks of dual-antiplatelet therapy. Following a newly placed bare metal stent, noncardiac surgery should be scheduled at least 30 to 45 days after the stent placement to decrease cardiac morbidity (179). Hemodynamic Monitoring Hemodynamic monitoring is integral to the perioperative management of patients with cardiovascular and pulmonary diseases. The major impetus for this advancement resides in the need for the quantitative estimate of cardiac function, resulting in the development of bedside pulmonary artery catheterization. The impact of monitoring cardiac function is demonstrated by the significant reduction of myocardial infarctions in high-risk patients who are aggressively monitored for 72 to 96 hours postoperatively (175).
Protein Interpectoral nodes as the initial site of recurrence overexpression and gene amplification of c-erbB-2 in breast cancer symptoms viral infection cheap neurontin 300 mg with amex. Loss of the hybridization of formalin-fixed in treatment discount 600mg neurontin amex, paraffin-embedded tight junction protein claudin-7 correlates with tissues symptoms thyroid cancer cheap neurontin american express. Not histological grade in both ductal carcinoma in situ eligible outcomes and invasive ductal carcinoma of the breast medications 24 discount neurontin express. Detection eligible target population of K-ras gene mutations at codon 12 in the 1389 treatment vaginal yeast infection best neurontin 800mg. Morphological pancreatic juice of patients with intraductal observations regarding the origins of atypical cystic papillary mucinous tumors of the pancreas medicine man order cheap neurontin line. Multifocal ras and p53 gene mutations in tissue and pancreatic intraductal papillary adenocarcinoma of the juice from pancreatic adenocarcinomas. Not eligible target population of breast-conserving therapy for ductal carcinoma in 1405. Breast Cancer Res Treat 2001 Jun; focal hypermetabolic activity in the breast: 67(3):245-53. Not eligible target population Expression analysis of carbohydrate antigens in 1396. Clinical and ductal carcinoma in situ of the breast by lectin radiological predictors of complete excision in histochemistry. Breast of liquid-based preparation to fine needle aspiration duct micro-endoscopy: a study of technique and a B-54 morphological classification of endo-luminal Cancer 2003 Apr 25; 99(2):97-104. Perioperative interstitial irradiation in the Paget disease of the nipple: a multifocal conservative management of early breast cancer. Early national trends over a decade in the surgical stage breast cancer: local control after conservative treatment of ductal carcinoma in situ. Am J Surg surgery and radiation therapy with immediate 2003 Dec; 186(6):723-8; discussion 8-9. Breast localisation biopsy of non-palpable breast lesions: conservation therapy with tumor bed irradiation reasons for unsuccessful excision. Eur J Gynaecol alone in a selected group of patients with stage I Oncol 2006; 27(3):262-6. Expression of P Not eligible target population cadherin, but not E-cadherin or N-cadherin, relates 1430. Not eligible target population putative cytokine highly expressed in normal but 1419. Proc Natl organizer regions in intraductal lesions associated Acad Sci U S A 2001 Aug 14; 98(17):9796-801. Not eligible target Detection of breast cancer in nipple aspirate fluid by population CpG island hypermethylation. Not eligible needle aspiration cytology of cystic hypersecretory outcomes ductal carcinoma in situ of the breast: a case report. Am J Surg 2006 Oct; 192(4):520 breast cancer pathology reporting in Australia in 4. Tubular carcinoma eligible outcomes and grade 1 (well-differentiated) invasive ductal 1425. Significance of flat epithelial outcomes atypia on mammotome core needle biopsy: Should 1452. Not eligible target risk factors associated with bilateral breast cancer in population area with early age diagnosis but low incidence of 1453. Breast Cancer Res screen-film mammography with respect to Treat 2006 Sep; 99(2):221-8. Not eligible target diagnostic accuracy of lesion characterization in population breast tissue biopsy specimens. Ned Tijdschr Predictors of surgical margin status in breast Geneeskd 2008 Nov 15; 152(46):2512-3. Annals of Surgical Oncology 2008 Sep; Mammographic screening in women at increased 15(9):2542-9. Not cytokeratin expression in relation to biological eligible target population factors in breast cancer. Not eligible Frequency of local recurrence following tylectomy outcomes and prognostic effect of nuclear grade on local 1447. Not Histopathological assessment of anastrozole and eligible level of evidence tamoxifen as preoperative (neoadjuvant) treatment 1460. J Cancer Res Clin Oncol 2008 Jun; invasion, multicentricity, lymph node metastases, 134(6):715-22. Not eligible level of evidence factors for breast recurrence in premenopausal and 1461. Cancer 1990 Apr 15; cases without or with minimal extent of underlying 65(8):1867-78. Not eligible target population Clinicopathological characteristics of atypical cystic 1462. Pathol Int 2000 Oct; with loss of heterozygosity on chromosomes 16q 50(10):793-800. Int J Radiat Oncol Biol Phys 1993 Jun neoplasia in a patient with pituitary acromegaly. Mod Pathol 2002 Dec; immunohistochemical study of the presence of c 15(12):1318-25. Not pancreatectomy for ductal adenocarcinoma of the eligible target population pancreas with special reference to resection of the 1465. World J Surg carcinoma of the breast: a review of 9 cases, with 1993 Jan-Feb; 17(1):122-6; discussion 6-7. Correlation of needle biopsy: study of 52 biopsies with follow-up c-erbB-2 protein expression with histologic grade, surgical excision. Not lymph node involvement and steroid receptor status eligible outcomes in human breast tumors. Annals of Surgical Oncology component: correlation of the histologic type of the 2008 Sep; 15(9):2556-61. Not eligible level positive breast carcinoma: prolonged survival with of evidence combined chemotherapy and trastuzumab. Diagnosis and Prognostic value of histologic grade nuclear management of male breast cancer. Not eligible target An improved score modification based on a population multivariate analysis of 1262 invasive ductal breast 1471. Not (encysted) papillary carcinoma of the breast: a eligible outcomes clinical, pathological, and immunohistochemical 1472. Apocrine target population ductal carcinoma in situ of the breast: histologic 1473. Quantitative analysis of allele imbalance supports Hum Pathol 2001 May; 32(5):487-93. Not eligible atypical ductal hyperplasia lesions as direct breast outcomes cancer precursors. Tumour Biol 2004 Jan-Apr; histopathologic importance of identification with 25(1-2):14-7. Inflammatory infiltrate in invasive lobular and B-57 ductal carcinoma of the breast. Clin Imaging 1999 years and younger: long term outcome for life, Nov-Dec; 23(6):339-46. Not carcinoma in situ diagnosed with stereotactic core eligible level of evidence needle biopsy: can invasion be predictedfi Not eligible screening of the contralateral breast in patients with outcomes newly diagnosed breast cancer: preliminary results. Not eligible breast cancer in a small peripheral New Zealand target population hospital. Mucinous metaplasia of breast eligible target population carcinoma with macrocystic transformation 1494. A case of diode laser eligible exposure photocoagulation in the treatment of choroidal 1496. Radiology 2008 Mar; 246(3):763 breast and its variants: a clinicopathological study 71. Quantitative Not eligible level of evidence promoter hypermethylation profiles of ductal 1511. Quantitative tumor of the breast associated with ductal assessment of promoter hypermethylation during carcinoma in situ and mucinous carcinoma: a case breast cancer development. Histopathology 2007 Jun; Journal of surgical oncology 2008 Jul 1; 98(1):15 50(7):859-65. Dual-energy role of Tc99m-sestamibi scintimammography in contrast-enhanced digital subtraction combination with the triple assessment of primary mammography: feasibility. Case Analysis of intratumoral heterogeneity and report: complete lymphatic staging in breast cancer amplification status in breast carcinomas with by lymphoscintigraphy and sentinel node biopsy. The stereotactic fine needle aspiration biopsy and role of magnetic resonance imaging in the stereotactic core needle biopsy in ductal carcinoma assessment of local recurrent breast carcinoma. Relationship operative simultaneous stereotactic core biopsy and between long durations and different regimens of fine-needle aspiration biopsy in the diagnosis of hormone therapy and risk of breast cancer. Clonality analysis of quantization help to evaluate small mammographic intraductal proliferative lesions using the human lesionsfi Independent mannose-6-phosphate/insulin-like growth factor 2 validation of candidate breast cancer serum receptor coded by a breast cancer suppressor genefi Proc Natl Acad Sci U S A 2008 Nov 18; Not eligible target population 105(46):17937-42. Expression cyclooxygenase-2 expression in ductal carcinoma in of parathyroidlike protein in normal, proliferative, situ lesions and invasive breast cancer correlates to and neoplastic human breast tissues. Am J Pathol cyclooxygenase-2 expression in normal breast 1993 Oct; 143(4):1169-78. Pathology & Laboratory Medicine 2009 Jan; Percutaneous large-core biopsy of papillary breast 133(1):15-25. Atypical ductal hyperplasia diagnosed at stereotaxic Anticancer Res 1999 May-Jun; 19(3B):2275-9. Not core biopsy of breast lesions: an indication for eligible outcomes surgical biopsy. Can large trial experiences be Recurrent carcinoma after breast conservation: reproduced in a community hospital settingfi Not eligible target Percutaneous removal of malignant mammographic population lesions at stereotactic vacuum-assisted biopsy. Not eligible Calcification retrieval at stereotactic, 11-gauge, outcomes directional, vacuum-assisted breast biopsy. Not eligible needle biopsy of synchronous ipsilateral breast outcomes lesions: impact on treatment. One Epithelial displacement after stereotactic 11-gauge operation after percutaneous diagnosis of directional vacuum-assisted breast biopsy. Ann Surg Bracketing wires for preoperative breast needle Oncol 2009 Jan; 16(1):106-12. Correlation of mammographic appearance or to sample the mammographic target: what is the and molecular prognostic factors in high-grade goal of stereotactic 11-gauge vacuum-assisted breast carcinomas. Probably study of conservative surgery without radiation benign lesions at breast magnetic resonance therapy in select patients with Stage I breast cancer. Borderline eligible outcomes breast lesions diagnosed at core needle biopsy: can 1553. Aspects of early stages, progression and receptor downregulates E-cadherin gene expression related problems. Comparison age at first childbirth on risk of developing specific of loss heterozygosity in primary and recurrent histologic subtype of breast cancer. Flow Her-2/neu level predicts decreased response to cytometric and histological analysis of ductal hormone therapy in metastatic breast cancer. Cancer Res more likely than women from the United Kingdom 1982 Aug; 42(8 Suppl):3434s-6s. Breast improved prognosis for patients with T1N0M0 Cancer Res Treat 2008 Mar; 108(2):271-7. Cancer 2006 evaluation of residual disease in women receiving Nov 1; 107(9):2245-53. Role of reconstruction using the superior gluteus for free ultrasound and sonographically guided core biopsy tissue transfer: a case report. J La State Med Soc in the diagnostic evaluation of ductal carcinoma in 1988 Jun; 140(6):43-5. Tumori 2000 activation, normal T cell expressed and secreted Nov-Dec; 86(6):A13-8. Not eligible exemestane administered for 2 years versus placebo outcomes on bone mineral density, bone biomarkers, and 1614. Opportunistic patterns of allelic loss in estrogen receptor-positive breast cancer screening in Hong Kong; a revisit of infiltrating lobular and ductal breast cancer. Changes in incidence of reduction mammaplasty in reconstructing partial in situ and invasive breast cancer by histology type mastectomy defects. Megestrol Immediate endoscopic latissimus dorsi flap: risk or acetate versus aminoglutethimide for metastatic benefit in reconstructing partial mastectomy defects. N cytokeratin 7 expression is not restricted to Paget Engl J Med 1982 Oct 14; 307(16):1010-4. Not cells but is also seen in Toker cells and Merkel eligible target population cells. Experience with fine-wire localization breast Mammary gland anatomy and the role of biopsies for nonpalpable breast lesions detected mammography and ultrasonography in the early mammographically.
Syndromes
- "Water pills" (diuretics) to get rid of extra fluid
- A ureteral stent (tube that allows the ureter to drain into the bladder)
- Fluids through a vein (IV)
- You have not had any bad outcomes during an earlier pregnancy.
- Have unusual distress when routines are changed
- Have you recently changed your diet?
D medicine hat news buy neurontin visa, if the child is older medicine organizer neurontin 800 mg otc, the leg may be slightly shorter shinee symptoms purchase 300 mg neurontin with visa, and the hip externally rotated medicine for depression discount neurontin 400mg without a prescription. G symptoms zoloft dose too high buy genuine neurontin, if the child has been walking treatment xanax withdrawal buy generic neurontin canada, lumbar acetabula: the abnormal femoral head lies lateral to the vertical and lordosis may be increased. B, where the acetabular roof is defective, Examination, Churchill Livingstone 1988, permission requested. A child with Perthes disease is aged 4-10yrs (occasionally 2-18yrs), and is usually male. If he presents early, he does so with intermittent episodes of pain in the front of the thigh, knee or groin, and a limp; in the early stages he is normal between these episodes. Sometimes there is no limp, but only some minimal abnormality of the gait, such as a tendency to walk with the leg turned inwards. Usually (but not always) all movements of the hip are mildly limited by discomfort rather than by pain, especially abduction and internal rotation. If movements are limited, the child usually also has spasm, particularly in the adductor and psoas muscles. If presentation is late, after the disease has run its course, the only signs may be a slight loss of the normal range of abduction, extension, and medial rotation of the hip, or he may have no symptoms or signs. If a good range of movement is particularly important, as in societies where people squat, an unstable mobile hip may be preferable to a stiff one, whatever the risk of later arthritis. If reduction is difficult or impossible, consider other causes of dislocation: (1) Partly treated septic or tuberculous arthritis. If you recognize this condition, do not attempt reduction, which may be impossible. If groin pain & vomiting persist, think of the rare Narath type of femoral hernia which is not visible clinically, but results in early bowel strangulation. C, abnormal side showing the head of the femur is smaller and denser, and the joint space looks increased. F, continued normal growth, whilst G, the head becomes wide and flattened on the abnormal side. Sequestration None fi to fi <fi normal Total (2),All or part of the head of the femur looks abnormally of head bone only dense, which indicates reduced vascularity. The cartilage Epiphysis Some lytic Significant Marked Collapsed surrounding it does not die; instead, it continues to enlarge, areas increased increased with radiodensity density mushroom and makes the joint space appear larger. The older he is, and the is <7yrs, unless risk factors are present when a femoral or more misshapen the head, the worse the prognosis. Unlike in slipped crutches and analgesics for 1yr is useful in the femoral epiphyses, the involvement of both hips is unusual co-operative child: add active hip exercises, folic acid and in Perthes disease (15% of cases, mostly in younger aggressive antibiotic treatment for staphylococcus or children). Lay the child supine, place your hands Remember also the possibility of disease near the hip on the affected thigh, and roll it backwards and forwards. Rotate the leg Suggesting transient synovitis: no radiographic changes, inwards and outwards. Rotation is usually more limited spontaneous resolution in a few weeks without further than abduction or adduction. If a radiograph is good, you may see when he flexes one of the digits it locks, and he cannot displacement of the fat shadow, or a widened joint space, extend it again, until he does so passively and forcefully, indicating fluid in the hip joint. The powerful flexors are more difficult to distinguish clinically and by radiography. Bone erosion around the If injection is not successful (50% of cases), apply a acetabulum (appearing to enlarge upwards), often with tourniquet and get fine instruments. Use a fine tenotomy knife to make a longitudinal incision in the sheath to release the tendon. Suggesting rheumatoid arthritis: from childhood to Leave the sheath open, suture the skin only, and start 40yrs (at the onset). Flex the wrist over the edge of a table; this will carefully: some children develop Perthes disease later. Moreover, if you fail surgically to remove a ganglion this is a chronic benign condition, in which the tendons no completely, it is more likely to recur, and if you dissect too longer run smoothly in their sheaths. If the patient complains of pain (and sometimes an If you have to explore for a ganglion, because you cannot abnormal prominence) over the radial styloid, which may rupture it, use a tourniquet, and remove some tendon be worse on extending and/or abducting the thumb, sheath with the ganglion, trying if possible to keep the cyst its abductor and short extensor tendons are constricted in of sticky synovial fluid inside the ganglion intact. The median nerve passes through the carpal tunnel on the palmar side of the wrist. It causes: (1);Pain, paraesthesiae and reduced sensation in the distribution of the median nerve (her thumb, the index and the middle finger, and the radial side of the ring finger). C, median nerve with an annular passes medial to the anterior superior iliac spine, and so constricting ring round it, caused by pressure from the edge of the may be entrapped under the inguinal ligament. Hang the arm up on a support, and watch the (1) Wasting of the muscles of the thenar eminence. Incise longitudinally for 4cm in the thenar crease, and then transversely for 2cm in the wrist crease. A patient with leprosy can lose feeling in the hands Look for the median nerve, but do not injure it! When this happens, neglected bruises, blisters, anteriorly, which is the site of pressure. Do not close the and cuts cause scars that progressively destroy the pulps of deep tissues. Persuade him that it is the injury to the hands which leads to wounds, and not the disease itself. If he fails to care for the fingers, and presents you with a severely disabled hand, there is little you can do, except to maintain such mobility as there is with physiotherapy. Patients are usually able to use their deformed hands quite well, and do not like having their fingers amputated. Tendon transfers and arthrodeses are sometimes helpful, and you can make a Z-plasty to widen the web of the thumb, but these are not easy operations. Ensure that all the joints of the hand are put through their full range daily, using the exercises (32-37D,E). If the ulnar nerve is acutely involved, rest the arm in a sling with the elbow at 90fi, and put the whole arm through its full range of motion at least once a day. If the lumbricals are involved, there is danger of development of a claw hand, so teach the exercises described (32-37F,G). If paralysis is chronic and slowly progressive, recovery is unlikely, so insist on exercises (32-37A): a paralysed hand is more useful if it is mobile rather than Fig. The first complaint making sure he wears protective gloves, or by adapting the may be painful glands in the axilla. If he smokes the pain which prevents a normal person from using the (persuade him not to) he must use a cigarette holder. Make sure that the insensitive hands are soaked and oiled So make sure that a leprosy patient rests an infected hand, in the same way as the feet (32. Apply it in the position of safety with the mcp joints flexed, If the flexor surface of the finger cracks, the ip joints almost fully extended, and the thumb do not let it heal with a short scar which will be likely to abducted, as if holding a tennis ball. Rest is essential: antibiotics on their own Use plaster strengthened with a stiff longitudinal wire, are inadequate. Observe the finger If infection starts as a macerated skin crease in a carefully for blueness. Initially, remove splints at night, paralysed finger, splint it with a posterior splint in just until you are sure they are not occluding the circulation. If the dorsum of the hand is scarred, so that the mcp If there is any discharge, add an antibiotic. This can happen as the result of a lepra reaction, If there is septic tenosynovitis, it is likely to be the result when a thick sheet of inflammatory tissue scars and of spread from a pulp infection. If there is one or more severely deformed fingers, If you feel rough bone at the base of an ulcer or sinus in such as a terminal phalanx bent to 90fi, the hand and pus oozes from a joint, this is osteomyelitis consider amputation or, better, an arthrodesis with or septic arthritis. If you feel rough bone at the bottom of a sinus over the tip of the finger, this is osteomyelitis of the terminal If the little finger is badly deformed, remove it with half phalanx. Splint the hand and fingers as nearly as possible If the septic arthritis does not heal, excise the joint. Immobilize the infected joint for at least and any dead tissues, and splint the joint in a position of 4-6wks after the infection is controlled, and the ulcer function (7. Pack the cavity that remains, and allow it healed, while putting all the other joints through their full to heal by granulation. If splinting one finger is position of function, and wait 12wks till the joints are no difficult, you may be justified in splinting it with one of its longer painful. One of the hazards of a shoe is that it may press on the sides of the big toe over a long period, and make the side of the nail grow into the soft tissues and cause pain, inflammation, and the discharge of pus from the nail fold. Carefully cutting away the nail may relieve the symptoms, but if this fails, more radical surgery is indicated. If the toe-nail is not deformed, you can excise a wedge of soft tissue; but if it is deformed, a more comfortable toe will result if you remove the whole toe-nail, including its bed. If the nail grows back in the same way, you can again remove a wedge, including a wedge of the nail bed. A tourniquet gives a bloodless field: you can achieve this with a rubber twisted around the base of the toe. Do not do this operation if there is peripheral vascular disease; use prophylactic antibiotics with diabetics and advise elevation for 24hrs. The exercises shown here are for acute and chronic paralysis, and will prevent a hand like (B) from becoming a stiff claw hand (C) which physiotherapy cannot cure. E, Use your other hand to rub your fingers as straight as they will go, taking care not to crack any weak skin. H, Use your other hand to straighten the end joint of your thumb, as straight as it will go. I, Pull gently and firmly, as if you were trying to lengthen your thumb, but do not pull it backwards. K, then straighten the end joint of your thumb as firmly nail bed and then close the wound. When sepsis has settled, remove the entire germinal matrix (the growth plate) of the nail. Make sure the nail has been removed; use a tourniquet and (2) Later, osteomyelitis produces a periosteal reaction. Make two 1cm incisions proximally from the (3),Chronic osteomyelitis causes dense sclerosis, corner of the nail to the transverse skin crease over the ip often with sinuses, and usually involves an extensive area joint (32-38A). Close (6) simple bone cysts & exostoses, the wound with 3/0 monofilament sutures after removing (7) metastatic tumours, and other primary bone tumours. The tumour extends considerably beyond the area of the bone, which is involved clinically, Primary tumours of bone are unusual, and have a or radiologically. There are: osteosarcomas, metastases, and these occur in 20% within 6 months if you mostly in the 10-25yr age group, chondrosarcomas perform an amputation alone. Fibrosarcomas arising from the chemotherapy: if there are no metastases, amputate if this periosteum behave like fibrosarcomas of the soft tissues. Remember a malignant the femur (the lower rather than the upper end, 20%), the bone tumour may be well vascularised, so use a tourniquet ribs (10%), and the skull and facial bones (10%). Try to avoid the disaster of Most arise de novo, but about 20% arise in patients with a pathological fracture or excessive bleeding after a multiple chondromas, and <5% from patients with a biopsy, or obtaining an unrepresentative sample. They are less aggressive than Remember to supply full details as well as radiographic osteosarcomas, and spread by local infiltration; films to the pathologist. Pelvic masses are hidden by the osteosarcomas; they occur either in teenagers, or rarely as overlying tissue, and present late. An osteosarcoma usually presents as a painful swelling or Cortical destruction is late, and periosteal reaction is pathological fracture of the metaphysis of the lower femur limited. The common sites are the epiphyses around the than the primary tumours of bone, and causes widespread knee (femur, tibia and fibula 50%) the lower radius (15%), osteolytic lesions in any bone, particularly the vertebrae, the pelvis and sacrum (12%), and the maxilla (29. When extraosseous lesions occur, They consist of giant cells (like osteoclasts) and they are usually formed by tumour growing from a bone. First they 40 & 70yrs, presents with bone pain, especially in the back expand the cortex, and then they spread through it. Lymphatic spread is rare, and distant metastases unusual, He may also have anaemia, renal impairment, but local recurrence after inadequate excision is common. After curettage the 5, 10, and 35yr survival rates are 45%, (2) Increased immunoglobulins in the blood (95%). It consists of densely packed small addition to aspirating it, because tumour cells are usually round cells. Melphalan or cyclophosphamide with prednisone increase the average survival from 17-52 months. If there are congenital constrictions of one or more Treat anaemia by transfusion. Treat infection of the chest limbs (rare), they are probably due to compression by and urinary tract. A scar is formed which leads to possible, or worthwhile, in relation to other problems. The limb may become ischaemic, paraplegia from spinal deposits, amyloidosis and because the constricting tissue does not grow.
300mg neurontin with amex. HIV - AIDS - Symptoms and Treatment - Part 4/7.
References
- Martinet N, Alla F, Farre G, et al. Retinoic acid receptor and retinoid X receptor alterations in lung cancer precursor lesions. Cancer Res 2000;60:2869-75.
- Wen JG, Yeung CK, Djurhuus JC: Cystometry techniques in female infants and children, Int Urogynecol J 11(2):103-112, 2000.
- Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med 2002;26(Suppl 4):S15-20.
- Price D, Milling L, Kirsch I, et al. An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. Pain. 1999;83:147-156.