Craig M. Misch, DDS, MDS
- Clinical Associate Professor, Department of Implant Dentistry
- New York University College of Dentistry
- New York, New York
- Private Practice - Oral and Maxillofacial Surgery and Prosthodontics
- Sarasota, Florida
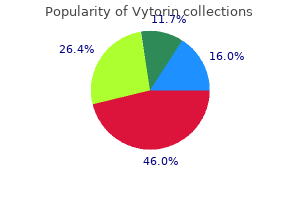
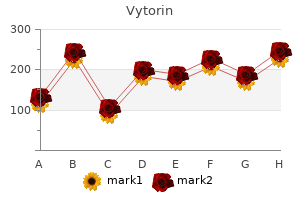
Three-dimensional analysis of active head and cervical spine range of motion: Effect of age in healthy male subjects cholesterol vs fat order vytorin 20 mg without prescription. Active range of motion utilized in the cervical spine to perform daily functional tasks cholesterol levels in eggs buy cheap vytorin 30 mg line. Differences in motor recruitment and resulting kinematics between low back pain patients and asymptomatic participants during lifting exertions cholesterol ratio us order genuine vytorin online. Trunkmusclestrengthinflexion cholesterol test monitoring system order vytorin online now,extension cholesterol en ratio order vytorin 20mg with mastercard,andaxialrotationinpatientsmanagedwithlumbardisc herniation surgery and in healthy control subjects cholesterol medication natural discount vytorin 30 mg online. Long-term flexion-extension range of motion of the prodisc: Total disc replacement. Moving centrally from the outer neurovascular capsule are fibrous annular plates, often erroneously called rings (they do not circle the disc). Because the number of anterior and lateral plates is greater than the number of posterior plates, the nucleus in the lumbar spine is positioned slightly posteriorly within the disc. Between the fibrous outer annulus and the inner fluid nucleus is a transition zone consisting of a loosely arranged collection of fibrous tissue that is highly deformable and acts as a buffer between the nucleus and annulus. The nucleus pulposus is a mucoid protein that binds approximately three times its weight in water and allows for distribution of forces. Rather surprisingly, because of its extensive water content, the disc is not a shock absorber. The functions of the intervertebral disc include the following: (1) It provides space and position for the segment to allow for the nerve root to pass through the foramen without compromise. Side lying or lying on the back with the knees bent and the back flat facilitates nutritional pressure changes. Therefore, by resting during the lunch hour and again at the end of the workday as well as at night, it is possible to more than double the nutrition to the disc. Side lying is of value if the knees are drawn up so as to flatten or slightly round the back. However, the moment the back assumes lordosis, it loads the posterior disc, restricting its ability to imbibe nutrient fluids through the cartilaginous end plate. Likewise, prone lying is not recommended unless there is a large, firm pillow beneath the abdomen to prevent the formation of lordosis. The recurrent sinu-vertebral nerve and a gray ramus communicans from the sympathetic chain innervate the disc. They penetrate the outer capsule and may extend as far as the second or third annular lamella. They noted the formation of a zone of vascularized granulation tissue from the nucleus pulposus to the outer part of the annulus fibrosus. Nerve growth was found deep into the annulus fibrosis and nucleus pulposus following the zone of granulation tissue in painful discs. Immunoreactive nerve fibers (such as substance P, neurofilament 2000, and vasoactive intestinal peptide) were more extensive in painful discs than in control discs. Annular tears noted at the periphery of discs were associated with this increased vascular granulation tissue, and these fibers may be the source of discogenic low back pain. What are some of the anatomic structures associated with mechanical dysfunction of the facet joint, and how might they be a source of mechanical pain With regard to the facet joint, there are five common conditions that can lead to pain and disability. The strained joint is painful, which causes its muscles to act as involuntary stabilizers, holding the joint against unguarded motion to facilitate initial healing. However, if the joint is held in this position for more than 1 or 2 days, because of pain or the fear of pain, the cross fibers of collagen in the capsule will begin to create capsular stiffness, resulting in a capsular pattern or restriction. Additionally, if there were a hemarthrosis present, adhesion can be expected to form from the fibrinogen in the resolving blood clot. In fact, any movement toward the pain that slides the superior facet downward seems to cause acute discomfort. The fact that an isometric contraction of the multifidus muscles or a rotation, gapping technique can often produce immediate relief tends to support this hypothesis. Thisshouldbe considered mostly a ligamentous condition, although laxity of the facet capsules may play a small role. However, they may also be the primary source of pain after unaccustomed overuse (eg, the first day of spring gardening). The most common cause of initial low back pain would be injury of the facet joints, followed by ligamentous weakness, sacroiliac strain, and ligamentous pain from the outer annulus. Pain may also develop from ligamentous instability in an unstable segment that is often adjacent to a stiff segment. Only in the area of acute low back pain (with no specific diagnosis) have satisfactory outcomes been established. The treatments determined to be effective were, in descending order, manipulation, patient instruction, and exercise. Based on a systematic review of the evidence, spinal manipulation performed by physical therapists is safe and resulted in improved clinical outcomes for patients with low back pain. How does a therapist determine when manipulation of the spine for mechanical low back pain is indicated Several researchers have found nerve endings in the outer two to three layers of the disc. Furthermore when the disc degenerates to the degree that it becomes engorged with blood vessels in an effort to repair the disc, sympathetic nerves accompany the blood vessels. Early back pain, particularly that associated with developing instability, is mostly from the disc, is usually felt in the back and buttocks, and is of a deep and vague nature, often poorly localized. When the disc herniates, one source of pain may be from the mechanical strain on the outer fibers of the annulus. If the prolapse places pressure on a nerve root, a sharper radicular radiating pain may pass from the back into the leg from compression of the dorsal root ganglia. With initial nerve root pressure, there is little pain because it appears that the nerves first have to become engorged and sensitized. Thus nearly 30 minutes may pass from the initial, sharp low back pain (tearing of the annulus) to the onset of radicular leg pain (pressure on the nerve root). Chemical irritation from inflammatory agents of the nociceptive fibers of the outer annulus may also cause pain. Discogenic pain is mediated by the sinu-vertebral nerves; it reaches the rami communicans through the L2 spinal ganglion. Does disc herniation result from weakness and damage to the annulus (outside in) or from pressure pushing the disc outward (inside out) Although the inner annulus may degenerate, tears begin at the outer annulus and spread inwardly, eventually allowing the nucleus to deform. The outer annulus is approximately three times as vascular as the capsule of the knee and thus can heal, as postmortem specimens have shown. Therefore, determining which patients have an outer annulus injury can aid in selection of the appropriate therapy to promote healing and prevent herniation. Glycosaminoglycan turnover within the annulus requires approximately 500 days; collagen turnover is even slower. The prevalence of lumbar disc prolapse usually occurs in the following order: L4/L5>L5/S1>L3/ L4>L2/L3>L1/L2. In the thoracic spine, what are the most common levels of dysfunction that present with clinical symptoms The junctional sites T1/2, T12/L1, and T4/5 are the most common levels of dysfunction. A direct relationship between the extent of the degree of facet tropism and the extent of disc herniation was not seen. Other studies by Hagg and Farfan found an unclear relationship between facet tropism and disc degeneration. The incidence of disc herniations cannot be answered for the simple reason that it is now believed that most disc herniations do not hurt. Neurologic signs arising from the lumbar spine most commonly occur in middle age, are more prevalent in men, and are typically a result of disc herniations, whereas neurologic signs arising from the cervical spine occur later in life, are more prevalent in women, and result from lateral foraminal stenosis caused by osteophytes from the lateral interbody, osteoarthrosis of the facet joints, and perhaps some disc material along with shortening and thickening of the ligamentum flavum. In 90% to 95% of patients, spinal pain (which often is disc-related) resolves in 3 to 4 months. Lumbar disc herniations are quite common, and most cases have a favorable prognosis. In Norway, Weber randomly denied surgery to half of the patients selected for surgery by good and fair criteria (not as liberal as in the United States). At the end of the first year, those who had surgery scored twice as well on assessment as those who did not. Surgery has not been determined to be more successful than conservative care, as indicated by guideline recommendations and published literature. In the past, studies of asymptomatic individuals have demonstrated that there is little or no correlation between low back pain and disc pathology. Other degenerative changes, such as radial fissures, end plate damage, and disc extrusions, have been linked with pain. Discuss the role of manipulation and manual therapy in the treatment of disc herniation. Manual therapy has no direct role in the reduction of disc herniations because neither traction nor manipulation has been shown to reduce the disc. However, manual therapy has been demonstrated to be effective by relaxing the muscles and allowing for movement in the segment. More physical techniques involving stretching and thrust may be of value at the neighboring stiff segments to increase motion and thus improve overall function of the spine, lessening the strain on the level with the disc herniation. For example, repetitive motion (eg, pendulum exercises) centralizes the pain to the shoulder, relaxes spasm, enables more motion, and hastens recovery. If the pain is from an intradiscal source, repetitive motion may alter the chemical balance. Extension places a higher stretch on the facet joint capsules than forward bending. Placing the hands in the small of the back and using them as a fulcrum mobilize the facet joints. Motion performed repetitively may reduce swelling around the nerve and thus the pressure that may cause ischemia. According to Panjabi, spinal range of motion can be divided into neutral and elastic-zone components. Instability is thought to occur when neutral-zone motion increases beyond normal (thus decreasing the elastic zone). Stabilization of the spine is thought to revolve around three subsystems: passive, active, and neutral. When either of these subsystems is impaired, aberrant movement can occur and lead to pain or disability. Rehabilitation should be directed at all three of these systems to increase function and decrease spine pain. The innervation of the facet joints is a branch of the posterior primary ramus, which supplies the skin and muscles to the back. A deep branch arises near the facet joint and innervates that joint, with a larger branch supplying the joint below and another branch traveling to the level above (perhaps only in the lumbar spine). The anterior innervation is by the recurrent branch of the sinu-vertebral nerve that arches over the intervertebral foramen to supply the ligamentum flavum and the anterior facet joint capsule. What muscles increase abdominal tone and pressure for stabilization of the lumbar spine The oblique and transverse abdominal muscles are important contributors to abdominal tone, while the multifidus muscle provides stabilization for the posterior spinal structures. The multifidus arises from the mamillary process just lateral to the facet joint and then passes upward and medially, attaching to the adjacent facet joint capsule and to the capsule above before inserting into the spinous process one and two levels above. Acting unilaterally, it tends to bend the spine to the same side and rotateit to the opposite side. Because the multifidus inserts into the capsules of the facet joints, it tends to pull the capsule out of the way, helping to prevent capsular impingement. As one of the deepest muscles in the back, it is considered to be a primary stabilizer. It is important that clinicians are able to target the multifidus when prescribing motor control exercises because it plays a significant role in lumbar stability. Decreased lumbar multifidus muscle activation is associated with the presence of factors predictive of clinical success with a stabilization exercise program.
Page 141 of 260 Anticonvulsants are also prescribed for other conditions that do not cause seizures cholesterol results chart vytorin 20mg fast delivery, including some psychiatric disorders (for antimanic and mood-stabilizing effects) and to lessen chronic pain cholesterol food chart download 30mg vytorin fast delivery. Small doses used for chronic pain are less likely to be associated with side effects that can interfere with safe driving than the doses used to treat other disorders cholesterol levels test range purchase vytorin in united states online. Waiting Period No recommended time frame You should not certify the driver until the medication has been shown to be adequate/effective cholesterol levels exercise discount 30mg vytorin with amex, safe foods raise good cholesterol naturally discount 30 mg vytorin otc, and stable cholesterol medication glass purchase vytorin 20mg without prescription. Recommend not to certify if: the driver uses anticonvulsant medications to control or prevent seizures. Episodic Neurological Conditions Episodic neurological conditions guidance can be grouped based on the type of risk associated with the condition. The first group considers the types of headache, vertigo, and dizziness that can affect cognitive abilities, judgment, attention, and concentration, as well as impact sensory or motor function sufficiently to interfere with the ability to drive a commercial motor vehicle safely. Page 142 of 260 the second group addresses the conditions that are known to cause or increase the risk for seizures, including epilepsy. In many situations, the occurrence of seizures is a reflection of the site of injury but may also be a surrogate for severity. Nonetheless, most neurological conditions in which acme or early seizures may occur are also risk factors for later unprovoked seizures. In fact, the occurrence of early seizures adds a significant increment of risk for later epilepsy to that associated with the primary condition. In general, the risk for subsequent unprovoked seizures is greatest in the first 2 years following the acute insult. Approximately 12% of individuals suffering an occlusive cerebrovascular insult resulting in a fixed neurological deficit will experience a seizure at the time of the insult. Unprovoked seizures will occur within the next 5 years in 16% of all individuals with an occlusive vascular insult. This rate seems not to be modified significantly by the occurrence of early seizures. The risk is increased primarily in individuals with lesions associated with cerebral cortical or subcortical deficits. The same risk of seizure and recommendations are applicable for intracerebral or subarachnoid hemorrhage. The length of time an individual is seizure free and off anticonvulsant medication is considered the best predictor of future risk for seizures. For those individuals who survive severe head injury, the risk for developing unprovoked seizures does not decrease significantly over time. Based upon the risk for unprovoked seizures alone, the driver should not be considered for certification. Individuals who have undergone such procedures, including those who have had surgery for epilepsy, should not be considered eligible for certification. Recommend not to certify if: the driver has a history of a severe brain insult with or without early seizures. In the presence of systemic metabolic illness, seizures are generally related to the consequences of a general systemic alteration of biochemical homeostasis and are not known to be associated with any inherent tendency to have further seizures. The risk for recurrence of seizures is related to the likelihood of recurrence of the inciting condition. Childhood Febrile Seizures Febrile seizures occur in from 2% to 5% of the children in the United States before 5 years of age and seldom occur after 5 years of age. From a practical standpoint, most individuals who have experienced a febrile seizure in infancy are unaware of the event and the condition would not be readily identified through routine screening. Most of the increased risk for unprovoked seizure is appreciated in the first 10 years of life. Therefore, the following drivers cannot be qualified: (1) a driver who has a medical history of epilepsy; (2) a driver who has a current clinical diagnosis of epilepsy; or (3) a driver who is taking antiseizure medication. Recommend not to certify if: the driver is taking anticonvulsant medication because of a medical history of one or more seizures or is at risk for seizures. Clearance from a specialist in neurological diseases who understands the Page 146 of 260 functions and demands of commercial driving is a prudent course of action if choosing to certify the driver with an established history of epilepsy. Consider headache frequency and severity when evaluating a driver whose history includes headaches. In addition to pain, inquire about other symptoms caused by headaches, such as visual disturbances, that may interfere with safe driving. Page 147 of 260 Monitoring/Testing You may on a case-by-case basis obtain additional tests and/or consultation to adequately assess driver medical fitness for duty. Single Unprovoked Seizure An unprovoked seizure occurs in the absence of an identifiable acute alteration of systemic metabolic function or acute insult to the structural integrity of the brain. While individuals who experience a single unprovoked seizure do not have a diagnosis of epilepsy, they are clearly at a higher risk for having further seizures. The overall rate occurrence is estimated to be 36% within the first 5 years following the seizure. After 5 years, the risk for recurrence is down to 2% to 3% per year for the total group. Following an initial unprovoked seizure, the driver should be seizure free and off anticonvulsant medication for at least 5 years to distinguish between a medical history of a single unprovoked seizure and epilepsy (two or more unprovoked seizures). The most common medications used to treat vertigo are antihistamines, benzodiazepines, and phenothiazines. Use of either benzodiazepines or phenothiazines for the treatment of vertigo would render the driver medically unqualified. Special consideration should be given to the possible sedative side effects of antihistamines. The medical examiner should determine if these drugs produce sedation in the individual driver. Aseptic meningitis is not associated with any increase in risk for subsequent unprovoked seizures; therefore, no restrictions should be considered for such individuals, and they should be considered qualified to obtain a license to operate a commercial vehicle. Follow-up You may on a case-by-case basis determine that annual medical examination is appropriate. Neuromuscular Diseases As a group, neuromuscular diseases are usually insidious in onset and slowly progressive. Rare neuromuscular diseases may be episodic producing weakness over minutes to hours. You must consider the effects of neuromuscular conditions on the physical abilities of the driver to initiate and maintain safe driving including steering, braking, clutching, getting in and out of vehicles, and reaction time. Examination by a neurologist or physiatrist who understands the functions and demands of commercial driving may be required to assess the status of the disease. Page 151 of 260 Autonomic Neuropathy Autonomic neuropathy affects the nerves that regulate vital functions, including the heart muscle and smooth muscles. Conditions Associated with Abnormal Muscle Activity this group of disorders is characterized by abnormal muscle excitability caused by abnormalities either in the nerve or in the muscle membrane. Follow-up the driver should have a biennial physical examination or more frequently if needed to adequately monitor medical fitness for duty. Congenital Myopathies Congenital myopathies are a group of disorders that may be distinguished from others because of specific, well-defined structural alterations of the muscle fiber and may be progressive or nonprogressive. Recommend not to certify if: the driver has a diagnosis of a congenital myopathy disorder. The severity can vary with the individual and in certain instances may be treatable or nonprogressive. Metabolic Muscle Diseases Metabolic muscle diseases are a group of disorders comprised of conditions affecting the energy metabolism of muscle or an imbalance in the chemical composition either within or surrounding the muscle. Conditions may affect glycogen and glycolytic metabolism, lipid metabolism, mitochondrial metabolism, or potassium balance of the muscle. Unlike most other neuromuscular disorders, these conditions may either be insidiously progressive or episodic. Recommend not to certify if: the driver has a diagnosis of a metabolic muscle disease. As a group these are debilitating, insidiously progressive conditions that interfere with the ability to drive commercial vehicles. Recommend not to certify if: the driver has a diagnosis of a motor neuron disease. Muscular Dystrophies Muscular dystrophies are hereditary, progressive, degenerative diseases of the muscle that interfere with safe driving. Recommend not to certify if: the driver has a diagnosis of a muscular dystrophy disease. In addition to limb muscle weakness, vision is often affected and easy fatigability is a common manifestation. Recommend not to certify if: the driver has a diagnosis of a neuromuscular junction disorder. Specialist may recommend a simulated driving skills test or equivalent functional test. Page 156 of 260 Peripheral Neuropathies this group of disorders consists of hereditary and acquired conditions where the nerves, including the axon and myelin or the myelin selectively outside the spinal cord, are affected. These conditions may affect the sensory or motor nerves individually, or both may be affected. You should evaluate the sensory modalities of pain, light touch, position, and vibratory sensation in the toes, feet, fingers, and hands for signs of peripheral neuropathy.
What is the difference between radicular referred symptoms and somatic referred pain accompanying a radicular disorder Radicular symptoms result from a block in conduction rather than nociceptive stimulation of pain sensitive structures (ie cholesterol in beer discount vytorin 30 mg with amex, the spinal nerve or nerve root) cholesterol check up fasting discount 20 mg vytorin free shipping. Radicular symptoms are typically referred to the distribution supplied by the involved spinal nerve or nerve root cholesterol medication at night purchase vytorin 30 mg on line, but this assumption must take into consideration the following: 1 cholesterol free eggs substitutes order vytorin online now. Radicular pain from a given nerve root does not always follow a consistent distribution cholesterol levels ketogenic diet purchase generic vytorin canada. Radicular symptoms do not always extend to the distal portion of the involved dermatome cholesterol in pasture raised eggs buy vytorin with visa. Somatic referred pain is generated by either mechanical or chemical irritation of somatic structures, such as the dural lining on the nerve root or the epineurium of the spinal nerve. Like radicular referred pain, somatic referred pain is felt in body regions separate from the irritated structures (eg, lumbar facet arthrosis can refer pain to the leg). Given the possibility of such disorders, the clinician must promptly screen patients at risk for such medical conditions and make the appropriate referrals. List common body systems and aggregates of signs/symptoms that may indicate systemic involvement. Women may experience pain referred into the right shoulder in addition to shortness of breath (sometimes occurring in the middle of the night) and chronic, unexpected fatigue. Silent attacks (painless infarction without acute symptoms) are more common among nonwhites, older adults (>75 years), smokers, and adults with diabetes (men and women), presumably because of reduced sensitivity to pain. For myocardial infarctions associated with a blood clot, what time frame for the administration of medications that dissolve clots, promote vasodilation, and reduce infarct size is considered the most crucial Administration of medication within the first 70 minutes after the onset of symptoms is associated with improved outcomes. However, angina pectoralis is less severe, does not last for hours (rarely more than 5 minutes), and is relieved by cessation of all activity and administration of nitrates. Pain in the chest lasting longer than 30 minutes, shortness of breath with exertion or when sleeping, increased fatigue, nausea, vomiting, nonproductive cough, nocturia, changes in skin color (blue or ashen), and onset of pain in the early morning hours are all cardiac red flags. Sharp, stabbing substernal pain, especially with exertion, pleural rub on auscultation, and referred upper trapezius and interscapular pain are symptoms of acute pleuritis. How does pulmonary function change with obstructive and restrictive pulmonary disorders Primary pain is typically noted over the midchest or involved lung and is often greater anterior as opposed to posterior. Referred pain may be noted in the neck, upper trapezius muscles, proximal shoulders, T1/C8 dermatome, along the ribs, and in the upper abdomen. What subjective questions should be asked when pulmonary dysfunction is suspected Musculoskeletal disorders mimicking pulmonary pain patterns include cervical radiculopathy (C8, T1), cervical and upper thoracic dysfunction (eg, arthrosis and spondylosis), rotator cuff disorders, and acromioclavicular arthritis regional muscle dysfunction (eg, pectoralis major strain, intercostal muscle strain, trigger points). What signs and symptoms are commonly associated with integumentary system pathology If edema is unilateral, consider a local or peripheral cause; if bilateral, consider a central disorder (eg, congestive heart failure and renal dysfunction). What subjective questions should be asked when integumentary system pathology is suspected About 40% to 50% of malignant melanomas arise from melanocytes in moles; the remainder arise from melanocytes in normal skin. Symptoms of shingles include vesicular eruptions and neuralgic pain in the cutaneous distributions supplied by peripheral nerves. Dysvascular Foot Ulcer Neuropathic Foot Ulcer Lesions are painful Lesions are painless Irregularly shaped Circular in shape Multifocal Develop over bony plantar regions Located on toes Can be associated with callous formation Located over nonplantar areas Tend to be clean and nonnecrotic Lesions are typically necrotic Ulcer regions are warm and pink Ulcer regions are typically cool and pale 34. Key characteristics include the following: poorly defined and widespread distribution that is red, edematous in appearance, and warm to hot with palpation; often accompanies infections. What is the most common intraabdominal disease referring pain to the musculoskeletal system Diseases affecting the esophagus can cause the following symptoms: 1) dysphagia (sensation of food catching in the throat), 2) odynophagia (pain with swallowing), and 3) a burning sensation beginning at the xiphoid and radiating to the neck and throat (heartburn). What signs and symptoms are commonly associated with stomach and duodenal pathologies Small intestine pain is described as cramping pain (moderate to severe in intensity), is intermittent in duration, and may be associated with nausea, fever, and diarrhea. What signs and symptoms are commonly associated with large intestine and colon pathologies Large intestine and colon pain is described as a cramping pain, dull in intensity, and steady in duration; it may be associated with bloody diarrhea, increased urgency, or constipation. Pancreatic pain is described as a severe, constant pain of sudden onset that is burning or gnawing in quality. Associated signs and symptoms include sudden weight loss, jaundice, nausea and vomiting, light-colored stools, weakness, fever, constipation, flatulence, and tachycardia; it may or may not be related to digestive activities. It is a point midway between the umbilicus and the right anterior-superior iliac spine used as a guide to locate the position of the appendix. The McBurney point is the most common site of maximum tenderness in acute appendicitis, which is typically determined by the pressure of one finger. Uremia, dizziness, headaches, heart failure, hypertension, ischemic lower extremity pain, muscle cramps, edema, peripheral neuropathy, weakness, decreased endurance, decreased heart rate, and decreased blood pressure and hypotension, among others 49. The costovertebral angle is the angle formed on either side of the vertebral column between the last rib and the lumbar vertebrae. Tenderness in this region is indicative of renal disease, and it is a potential site for unintended encroachment on the pleural cavity during surgery. What is a key feature that typically distinguishes a radicular disorder from renal pain Renal pain is rarely influenced by changes in spinal posture or movements of the spine. Hyperpigmentation, bruising, itching, paleness/anemia, redness of the eyes, shortness of breath, uremic breath, tremors, footdrop, weakness/altered movement patterns, decreased ability to concentrate, lethargy, irritability, and impaired judgment 53. Primary pain is typically noted in a T10 to L1 distribution, in the groin and genital regions. Pain is predominantly in the anterior, lateral, and posterior subcostal regions and posteriorly in the area of the lower costovertebral articulations. Common musculoskeletal disorders that mimic renal disorders include lower thoracic or lumbar plexus radiculopathy, lumbar and lower thoracic dysfunction (eg, arthrosis, spondylosis, and costal/costovertebral), regional muscle dysfunction (eg, adductor strain), central nervous system disease, meralgia paresthesia, and trauma. What musculoskeletal signs or symptoms may be associated with hepatic and biliary dysfunction Bilateral carpal tunnel syndrome accompanied by bilateral tarsal tunnel syndrome is a musculoskeletal sign associated with hepatic and biliary dysfunction. Pain associated with the liver, gallbladder, and the common bile duct is typically located in the midepigastric or right upper quadrant of the abdomen. Musculoskeletal pain referred from the hepatic and biliary systems may be located in the right shoulder, upper trapezius, or right scapular area or between the scapulae. What signs and symptoms are commonly associated with hepatic and biliary system pathologies In addition to the musculoskeletal pain referral patterns listed previously, patients experiencing hepatic or biliary dysfunction may also demonstrate changes in skin color, as well as neurologic symptoms. Skin changes include yellowing of the skin or sclera of the eyes (jaundice), pallor, and orange or green skin. Neurologic signs and symptoms include confusion, sleep disturbances, muscle tremors, hyperactive reflexes, and asterixis (flapping tremor where the patient is unable to maintain wrist extension with forward flexion of the arms). What subjective questions should be asked when hepatic and biliary system pathology is suspected Musculoskeletal conditions that may mimic hepatic and biliary pain patterns include symptomatic midthoracic hypomobility, rotator cuff dysfunction, and subacromial/deltoid bursitis. Erythrocytes Leukocytes Platelets Anemia Leukemia Thrombocytosis Aplastic anemia Leukocytosis Thrombocytopenia Hemorrhagic anemia Thrombocytopenia Hypochromic (iron deficiency) anemia Leukopenia Megaloblastic anemia Pernicious anemia Polycythemia Sickle cell anemia 65. History of headaches, blurred vision, dizziness, fainting, altered mentation, feeling of fullness in the head, altered sensation in the distal extremities, malaise, fatigue, weight loss, easy or unexplained bruising, cyanosis, digital clubbing, and hypertension 66. Alcoholism, burns, chronic pulmonary disease (eg, fibrosis), dehydration (eg, vomiting and diarrhea, burns, or use of diuretics), diminished blood-oxygen tension, heart disease (eg, cor pulmonale and congenital), liver disease, renal disease, smoking, and exposure to carbon monoxide 67. Signs and/or symptoms consistent with local or systemic infection (eg, fever) and inflammation or trauma 68. Burns, cancer, immune system responses (eg, lupus, rheumatoid arthritis), infections, inflammatory responses (eg, tissue damage), kidney failure, leukemia, lymphoma, malnutrition, multiple myeloma, removal of the spleen, stress (eg, emotional, physical), and tuberculosis 69. Pail skin and nails, shortness of breath with little to no exertion (based on degree), heart palpitation, and increased pulse rate; with severe anemia, fatigue, decreased diastolic blood pressure, and changes in mentation 70. What subjective information should be obtained when hematologic pathologies are suspected What are two primary life-threatening metabolic conditions that can develop if uncontrolled or untreated diabetes mellitus progresses to a state of severe hyperglycemia What two patient types may exhibit orthostatic hypotension because of slight dehydration, especially when intense exercise increases the core body temperature What signs and symptoms are commonly associated with endocrine system pathologies Neuromusculoskeletal signs and symptoms include muscle weakness, myalgia and fatigue, bilateral carpal tunnel syndrome, periarthritis, chondrocalcinosis, spondyloarthropathy, osteoarthritis, hand stiffness, and pain. What subjective information should be obtained when endocrine system pathology is suspected Periarthritis and calcific tendinitis of the shoulder is common in endocrine clients and must be ruled out from other musculoskeletal disorders such as rotator cuff dysfunction, rotator cuff tears, slap lesions, labral tears, and subacromial/subdeltoid bursitis. The four principal classifications are immunodeficiency, hypersensitivity, autoimmunity, and immunoproliferative disorders. Myasthenia gravis, Guillain-Barre syndrome, and multiple sclerosis are neurologic disorders associated with immune system dysfunction. Examples of autoimmune disorders are fibromyalgia syndrome, rheumatoid arthritis, systemic lupus erythematosus, scleroderma, spondyloarthropathy, Reiter syndrome, psoriatic arthritis, Lyme disease, and bacterial arthritis. What signs and symptoms are commonly associated with pathologies of the immunologic system What are other musculoskeletal causes of pain that must be differentially diagnosed from an immunologic disorder Because of the multisystem effect of immunologic disorders, it is important that a complete health history is performed to identify if musculoskeletal signs and symptoms are attributable to a mechanical origin, or whether other sources should be investigated. Close cooperation and appropriate co-management with the referring physician are crucial for the proper management of musculoskeletal cases with suspicious origins. Do knowledge, efficiency of data collection, and data interpretation improve with experience The literature suggests that inadequate knowledge and imprecise data collection improve with increasing clinical experience, but data integration and interpretation do not. It is well documented that human beings are for the most part noncritical thinkers and that we are prone to deductive and inductive errors in reasoning (ie, judgment errors). Additionally, the cognitive limitation of human working memory leads us to access simpler rather than more complex cognitive or problem-solving strategies (ie, shortcuts in reasoning). In actuality, it is likely that the combination of judgment errors and reliance on shortcuts in reasoning (eg, heuristics) is what leads to most errors in clinical reasoning. Finally, errors will vary based on the difficulty of the patient case, knowledge of content and context, strategy selection, and integration and interpretation of pertinent patient information. Deductive reasoning involves reaching a conclusion based on evidence (ie, deductive reasoning combines two or more pieces of evidence to reach a conclusion). Illogical or poor reasoning, persistence of beliefs despite empiric data to the contrary, rationalizing, justifying, and using biases and heuristics to assess information are examples of deductive reasoning errors. Inductive reasoning uses specific pieces of evidence (ie, more than one example) to draw conclusions that are probably, but not necessarily, true (eg, generalizations, cause and effect, and analogies). Examples include overconfidence in validity of beliefs, confusion of opinion or anecdotal evidence with truth, overestimation of knowledge, and basing a decision on personal interests. Iterative hypothesis testing, as described by Kasper and Harrison, is a process used by medical practitioners to increase the efficiency of the interview process. During this process interview questions are used to confirm or refute the evolving diagnostic hypothesis. Iterative hypothesis testing does not replace a systematic, thorough, and complete history of present illness, past medical history, review of systems, family history, and the physical examination. Iterative hypothesis testing represents a pattern of application of inductive and deductive reasoning.
Syndromes
- Wash linens in hot water (at least 130 degrees Fahrenheit) to kill dust mites
- Take the drugs your doctor told you to take with a small sip of water.
- Nausea
- Deformity of the chest
- You have severe fatigue and weakness
- How did this cycle (and others) differ from your usual menstruation?
- Cryoglobulins
- Whether it is cancerous
- Tantrums get worse after age 4
Neurosurgeons deal with disease processes that are unique to the central nervous system: Parkinson disease ldl cholesterol definition wikipedia buy cheap vytorin 20mg on-line, epilepsy cholesterol lowering diet books discount 20mg vytorin otc, developmental disorders cholesterol pills glass purchase vytorin no prescription, and even psychi atric disorders cholesterol enhancing foods best vytorin 30 mg. The surgical approach to this gamut of pathologies cholesterol normal lab values buy vytorin pills in toronto, as you might imagine cholesterol level in quail eggs discount generic vytorin canada, is also remarkably diverse. In a given week, a neurosurgeon may deli cately dissect out a brain tumor under the operating microscope, perform a spinal fusion with pedicle screw xation, and use minimally invasive stereotactic tech niques for surgery on a patient with Parkinson disease. They love being able to correct abnormalities of this organsystem by using their hands, sur gical instruments, and the latest operative technology. Witnessing this phenomenon for the rst time evokes ex traordinary feelings: exhilaration, fear, and empowerment all at the same time. Operating on the brain is a skill that requires brilliant manual dexterity, often making the difference between life and death. After making a diagnosis, close collaboration with neu rologists and neuroradiologists is implemented to provide the best patient care. Neurosurgeons deal with a wide variety of potentially debilitating brain diseases: traumatic brain and spine injuries, strokes, intracranial hemorrhaging from aneurysms and other vascular malformations, brain tumors in eloquent cortex, chronic back pain, sci atica, and even movement disorders such as epilepsy. The procedures are often long and intricate and require a high level of manual dexterity and stamina. Residency in neurosurgery is arguably the most physically and emotionally rigorous training in medicine. Those suffering from subarachnoid hemorrhages due to ruptured aneurysms may quickly deteriorate in the neurosurgical intensive care unit. This may happen, of course, at the same time the on-call resident has to evaluate the newest head trauma in the emergency department. In this eld of medicine, true emergencies require immediate attention that cannot wait until the next morn ing. Rapidly expanding blood clots in the brain or spinal cord can leave patients dead or paralyzed if not attended to urgently. In 1999, the American Association of Neurological Surgeons conducted a survey of 1570 neurosurgeons and found that 94% of the re spondents were men and 85% were Caucasian. Likes the immediate gratica Neurosurgeons do not, for the most part, tion of surgical outcomes. Keep in mind, however, that this can be true for any specialty, especially within the sur gical elds. The vast majority of neurosurgeons are kind, dedicated profession als who care about their patients (the sickest patients in the hospital more often than not). As a group, neurosurgeons are also very smart and technically savvy enough to adapt to the rapid advances in the surgical treatment of neurologic disease. Cerebrovascular Neurosurgery: Operating on the Blood Vessels of the Brain Cerebrovascular neurosurgery uses a surgical approach to treating vascular dis eases of the brain and spinal cord. Intracranial aneurysms, arteriovenous malfor mations, arterial dissections, and occlusions of the extracranial carotid arteries are just a few of the many disease processes with which the cerebrovascular surgeon is confronted. As you might imagine, virtually all vascular diseases of the central nervous system are serious and potentially deadly. Most neurosurgeons agree that vas cular surgery of the central nervous system is among the most technically chal lenging and delicate surgery done in the eld. Not long after Egaz Moniz in troduced cerebral angiography to the world, Normon Dott, a neurosurgeon, per formed what may have been the rst successful surgical attack on an intracranial aneurysm. Dott treated this aneurysm by wrapping the vessel with muscle, a tech nique still used for some large, unclippable aneurysms. This certainly was not the rule early in the early his tory of this subspecialty. A study done in 1965 suggested that the results of con servative therapy for intracranial aneurysms (no surgery) were actually better then if patients underwent surgical attack. The further development of modern aneurysm clips and microsurgical techniques over the ensuing decades by such neurosurgical legends as Drake and Yasargil maximized the surgical treatment of intracranial vascular disease pro cesses like aneurysms and arteriovenous malformation. In fact, some believe that the golden age of the cerebrovascular surgeon has passed, with the surgical treat ment of these diseases reaching its climax in the 1980s. In recent years, an entirely different approach to the treatment of neurovas cular disorders has been growing rapidly. Interventional neuroradiology, or en dovascular neurosurgery, is a relatively new eld approaching these disease pro cesses. These subspecialists make a small incision in the groin to access the femoral vessels, utilize a guide wire to travel into the intracranial circulation, and then perform cerebral angiography for visualization and navigation. Guglielmi detachable coils, which are used to treat intracranial aneurysms, perhaps best il lustrate an endovascular technique. In this procedure, a catheter is introduced into the femoral vein and advanced into the intracranial circulation until it reaches the aneurysmal lumen. At this point, platinum coils are dropped into the aneurysm until it appears that the aneurysm itself is completely packed, with no residual aneurysm and a patent parent vessel. Early studies suggest that the use of this promising technique is rapidly increasing. Some neurosurgeons be come pretty emotional when they get started in this conversation. At the present time, coiling techniques are still reserved for patients with poor-grade subarach noid hemorrhage and those with aneurysms located in especially delicate regions of the brain with increased surgical morbidity and mortality. These observations aside, the use of endovascular techniques in lieu of surgery is still institution de pendent. Does the rise of endovascular neurosurgery mean that the era of the surgical clip is coming to an end In the meantime, open surgical treatment of cere brovascular disease is alive and well. For those who love aneurysms, this does not necessarily mean that you should become a radiologist. In fact, many neurosurgeons are currently training in en dovascular fellowships after residency. As you might imagine, there are certainly advantages to being a neurosurgeon who can clip and coil an aneurysm with equal prociency. Neurosurgical Oncology: Cancer and the Brain In the United States, approximately 17,000 people per year are diagnosed with primary tumors of the brain. From a surgical perspective, the approach to brain tumors can be quite chal lenging. Tumors can arise from any location in the brain, and elaborate surgical planning is required. Anyone who has studied the anatomy of the head, neck, and brain understands the difficulty in gaining access to places such as the skull base, the sella turcica, and the posterior fossa. Complex dissections have been de veloped over the years such as transphenoidal approaches for tumors of the pi tuitary axis and translabrynthine approaches for tumors of the eighth cranial nerve (the vestibulo-auditory nerve). Unfortunately, limited success has been the rule in the surgical treatment of highly aggressive brain tumors. Sadly, systemic chemotherapy has been minimally ef fective in prolonging the lives of these patients. Given the active role that academic neurosurgeons play in developing this technology, many ther apies will likely become part of the neurosurgical therapeutic repertoire rather then the realm of neurologists or radiologists. Because of the hot research going on in this area and its direct application to clinical neurosurgery, neurosurgical oncology is a particularly appropriate eld for individuals with a bent for aca demics. This is an interesting statistic considering that, according to many older neurosurgeons, spine as a surgical eld was almost lost to the orthopedic surgeons in the not-so-distant past. As the aforementioned numbers suggest, the spine is now a major component of neurosurgery. Medical students interested in this specialty should be aware that a number of older surgeons make a distinction between ortho spine and neuro spine. The latter refers to patients with decompressions and other simple, more delicate spine procedures that are often done under the operating microscope. Ortho spine de notes spine surgery involving instrumentation, such as fusions and spinal defor mity operations. As it turns out, these distinctions were made by physicians who were neither orthopedic nor neurologic surgeons. There are neurosurgeons who do the larger spine whacks, including some who do multilevel fusions with complex instrumentation for scoliosis. On the other hand, there are orthopedic surgeons who quite adeptly perform decompressions under the operating microscope. No statistic exists that suggests whether orthopedic surgeons or neurosur geons are more suited or better prepared to operate on the spine. There are, nonetheless, several issues to consider if you want to be a spine surgeon and are trying to choose between orthopedics and neurosurgery. In general, neurosurgery residents tend to operate on the spine with greater frequency and earlier in their training then their orthopedic colleagues. Lumbar discectomies tend to be be ginner cases for neurosurgery residents because these procedures are considered less risky then craniotomies. At many teaching hospitals, a simple spine case in volving the lumbar region is usually the turf of the rst and second year neuro surgical resident. In contrast, orthopedic spine cases at the same institution are reserved for more senior residents. Furthermore, there are few orthopedic pro grams in the country where 60% of the cases done are spine related. It would have saved me a lot of sleep and years off of my life lost from the stress of neurosurgical training. Even if neurosurgery residents have an initial advantage in spine surgery because of their exposure and experience, it seems clear that orthopedic surgeons never fall that far behind. Fortunately, these two elds have enough differences overall that most physicians-in-training are able to gure out where they belong. Pediatric Neurosurgery: Bringing Hope to Smaller Patients Pediatric neurosurgery involves the surgical treatment of pediatric disorders of the nervous system. Obviously, there is some overlap between what adult and pedi atric neurosurgeons do. Although brain tumors occur in both children and adults, the natural history of these disease processes is often remarkably different. In this operation, a burr hole is made in either the frontal or occipital areas of the skull so that a catheter can pass into the ventricular system. Surgeons then attach the catheter to tubing tracked underneath the skin from the scalp to the abdomen. As in all neurosurgical subspecialties, new and exciting technological ad vances in pediatric neurosurgery are on the horizon. A particularly fascinating area is fetal neurosurgery, currently performed at only a few select institutions. In these cases, operative repair of congenital brain malformations in the early phase of human development may prevent progressive disability from secondary pathophysiology or from injury stemming from the intrauterine environment. Neural tube defects and fetal hydrocephalus are examples of the kinds of pathol ogy that are currently the focus of this developing area. Stereotactic and Functional Neurosurgery: Precise Mapping, Precise Treatment Stereotactic and functional neurosurgery is a particularly exciting area in neu rosurgery these days. This specialty is an especially good eld for technology buffs and for those who loved the intricate pathways of the brain memorized (and of ten forgotten) in medical school. The resulting images provide a virtual three-dimensional map for a variety of procedures to be performed. Based on this map, needles are precisely targeted to the desired location in the brain.
Vytorin 30mg visa. हार्ट की नालियों से कोलस्ट्रोल कम करने के सबसे असरदार उपाय.
References
- Chung P, Parker C, Panzarella T, et al. Surveillance in stage I testicular seminoma: risk of late relapse. Can J Urol 2002;9(5):1637-1640.
- Catto JW, Hartmann A, Stoehr R, et al: Multifocal urothelial cancers with the mutator phenotype are of monoclonal origin and require panurothelial treatment for tumor clearance, J Urol 175:2323n2330, 2006.
- Howe AS, Palmer LS: An inguinal approach to complex extravesical ureteral reimplantation, Urology 106:178n182, 2017.
- Fizazi K, Tran N, Fein L, et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med 2017; 377(4):352-360.
- Byar D, Blackard C: Comparisons of placebo, pyridoxine, and topical thiotepa in preventing recurrence of stage I bladder cancer, Urology 10:556n562, 1977.