Luis A. Tamara, MD
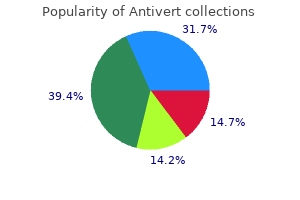
- Staff Nuclear Medicine Physician
- Division of Nuclear Medicine
- Veterans Administration Medical Center
- Bay Pines, Florida
One adult-strength multivitamin that contains iron medications prescribed for ptsd purchase antivert 25 mg overnight delivery, folic acid treatment quadratus lumborum buy generic antivert 25mg on-line, and thiamine (vitamin B1) daily treatment lyme disease order genuine antivert. A daily sublingual vitamin containing 500 mcg of vitamin B12 or a monthly injection of 1 medicine hat news buy antivert with amex,000 mcg of vitamin B12 symptoms week by week cheap 25 mg antivert amex. Calcium citrate containing 1 94 medications that can cause glaucoma buy discount antivert 25 mg line,200 to 1,500 mg plus vitamin D; it is suggested to take calcium in at least two dosages. Unfortunately, despite the convincing evidence supporting the use of simulation in surgical education, there is still a gap in translation of knowledge and technical skills from the research environment into clinically relevant training curricula. The objective of this thesis was to design and validate a comprehensive simulation enhanced training curriculum that addressed cognitive knowledge, technical and non-technical skill in laparoscopic bariatric surgery. The first study employed a modified Delphi methodology and an international panel of experts in surgical and medical education to develop a consensus-based framework for design, validation and implementation of simulation-enahnced training curricula in surgery. The second study used a modified Delphi methodology and an international panel of experienced bariatric surgeons to ii develop an objective scale for assessment of operative skill in laparoscopic gastric bypass procedure. This scale was feasible to use, had high inter-rater and test-retest reliability, as well as evidence of construct and concurrent validity. The third study used the previously developed consensus-based framework to design a comprehensive simulation-enhanced training curriculum for laparoscopic bariatric surgery. A prospective, single-blinded randomized controlled trial was used to compare the effectiveness of this curriculum in comparison to conventional surgery training. Surgery residents who were trained in this curriculum demonstrated superior technical skills, superior non-technical skills and enhanced safety in the operating room. Grantcharov for allowing me to pursue this opportunity, for his continued support, guidance and mentorship. Of the many things that I have learned from you over the years, the two that I will cherish the most are to never let a great opportunity pass by and to always remember which things are of real importance in life. Nicole Woods for their invaluable contributions as members of my thesis committee. Your helpful suggestions, keen attention to research methodology, constructive feedback and ongoing support were instrumental in raising the scientific quality of this work. Rajesh Aggarwal for his invaluable contributions as a research collaborator and a mentor. I was always amazed at the number of great research ideas that were generated at each of our meetings. Thank you for your ongoing support of my work, for always offering your help and most importantly for you friendship. I truly believe that we have many more years of productive research collaborations ahead. Andy Smith (Chair of the Division of General Surgery) for their support and the opportunity to engage in the Surgeon Scientist Training Program. I owe my deepest gratitude to my parents, Alexander and Natalia, for bringing me to the land of opportunities, for your continued encouragement, support, tremendous sacrifice and endless love. The following agencies provided operating grants in support of this work: Physicians Services Incorporated Foundation Resident Research Grant, the Education Development Fund for Innovation in Education, and Johnson and Johnson Medical Companies, Canada. All aspects of this body of work, including the planning, execution, analysis, and writing of all original research and publications was performed in whole or in part by the author. The following contributions by other individuals are formally and inclusively acknowledged: Dr. Grantcharov (Primary Supervisor and Thesis Committee Member) mentorship; laboratory resources; guidance and assistance in planning, execution, and analysis of studies as well as manuscript/thesis preparation Dr. Najma Ahmed (Thesis Committee Member) mentorship; guidance in planning of studies and thesis preparation Dr. Nicole Woods (Thesis Committee Member) mentorship; guidance in planning of studies and thesis preparation Dr. Rajesh Aggarwal mentorship; guidance in planning and analysis of studies for Section 1. Esther Bonrath assistance in planning, execution and analysis of studies for Chapters 3 and 4 Dr. Nicolas Dedy assistance in planning, execution and analysis of studies for Chapters 3 and 4 Dr. An evidence-based framework for the design of a simulation-based surgical training curriculum. Composition of the international expert panel for the online Delphi questionnaire. Agreement among the Delphi panel members for the 1 and 2 round of online Delphi questionnaire. Novice and experienced surgeons defined using the Objective Structured Assessment of Technical Skills Global Rating Scale criteria. This introduction is largely credited to Professor William Stewart Halstead during his time at Johns Hopkins Hospital, Baltimore, Maryland, United States (Rankin, 2006). In this model, surgery trainees were supervised by an attending surgeon and were offered a graduated level of responsibility as their training progressed. Most of the practice and training occurred on real patients in the operating room. This model of training has indeed produced many of the th outstanding surgeons of the 20 century; however, this approach to surgery training may no st longer be suitable in the 21 century in view of the minimally invasive approaches to conventional surgical procedures, reductions in resident work hours, decreases in the available operating room time, increases in the risks of malpractice litigation, increases in patient complexity and ethical requirements to protect patients from harm (Palter & Grantcharov, 2010). Simulation-based training has been proposed as a useful adjunct to conventional surgery training st to deal with some of these challenges that are facing surgeons of the 21 century (Torkington, Smith, Rees, & Darzi, 2000). Simulation-based training and practice in a simulation laboratory offers a number of advantages to a surgery trainee. It allows a trainee to practice a particular surgical task without any of the time pressures and inherent risks of training in the operating room. A trainee is allowed to make mistakes, correct them and try different approaches without any risk to the patient. He or she can become accustomed to various surgical instruments and can build the necessary dexterity for active participation in the operating room. An experienced attending surgeon can often notice that a novice surgery trainee is often not able to acquire new information or carry on a conversation in the operating room, while he or she is performing a basic surgical task. The explanation for this phenomenon centers on the availability cognitive resources at the time of performing a technical task (Figure 1). The cognitive resources of a novice surgery trainee are completely depleted by the technical task at hand, thus, he or she is not able to perform and engage in any other tasks in the operating room. Training in a simulation laboratory offers a novice trainee an opportunity to mature into a pre trained novice (Gallagher et al. A pre-trained novice is an individual who has been trained using simulation to the point where many of the psychomotor skills and spatial judgments have been automated and occupy fewer cognitive resources, allowing a novice trainee to focus more on higher level learning in the operating room (Figure 1). Following randomization, both groups had an introductory session on the basics of fascial closure. The simulation-based training group then practiced fascial closure to proficiency on an inanimate model, whereas the control group did not. At the completion of training both groups performed a fascial closure in the operating room, while listening to a verbal script that contained relevant clinical information. Participants in the simulation-based training group showed significantly greater technical skill in the operating room and knowledge on the multiple-choice test. Ericsson, deliberate practice is the key to expertise in professional sports, music, chess and medicine (Ericsson, 2008). Deliberate practice requires (a) a task with a well-defined goal, (b) motivation to improve, (c) provision of feedback, and (d) ample opportunities for repetition and gradual refinements in performance (Ericsson, 2008). Training on surgical simulators is well suited for deliberate practice as well defined goals can be set, feedback can be provided and multiple repetitions of a task can be performed at increasing levels of difficulty. Satava was one of the first to describe a virtual reality simulator for surgical skills training back in 1993 (Satava, 1993). Over the past 2 decades many different simulators were developed for use in technical and non-technical skills training. These include bench-top trainers, virtual reality simulators, models based on cadaveric tissues and live anesthetized animal models. They are frequently made from synthetic materials and allow for practice of surgical tasks such as suturing, tissue handling, Foley catheter insertion, chest tube placement and others. Bench-top trainers have also been used in the training and objective assessment of laparoscopic surgical skills. Such trainers often referred to as video-box trainers are made up of a box with multiple holes for placement of a laparoscopic camera and laparoscopic instruments. Synthetic and cadaveric tissues can be placed inside this box and various minimally invasive surgical skills (grasping, cutting, suturing, etc. Complex laparoscopic skills can also be learned and assessed using a video-box trainer with synthetic and cadaveric tissues. Bench-top trainers have a number of advantages and disadvantages in comparison to other training modalities (Munz, Kumar, Moorthy, Bann, & Darzi, 2004). Bench-top trainer advantages include low cost, versatility (can train on synthetic or cadaveric tissues), ability to use real instruments, and standardization of training. Bench-top trainers are also well suited for use in assessment of technical skills. The disadvantages of bench-top trainers include inability to simulate a complete operation, difficulties in adjusting the level of difficulty for deliberate practice, requirement for ongoing maintenance of equipment, and the requirement for presence of an experienced instructor for demonstration of skills and provision of feedback. Currently, there are simulators for basic laparoscopic tasks, advanced laparoscopic tasks, and procedural training in general surgery, orthopedics, otolaryngology, urology, vascular surgery and obstetrics and gynecology. The disadvantages include high up-front set-up costs, lack of realistic graphics and limited force feedback (Munz et al. The advantages of cadaver models include high fidelity, realistic anatomy and the ability to simulate entire operations. The disadvantages include high cost, limited availability, risk of transmissible infections, lack of bleeding, inability to simulate complications, and poor tissue compliance (Munz et al. The disadvantages in poor tissue compliance can be overcome with the use of Thiel human cadavers (Giger, Fresard, Hafliger, Bergmann, & Krahenbuhl, 2008), albeit such preparations make these models even more expensive. At the present time, training on human cadavers may be best reserved for advanced surgical skills and entire surgical procedures (Giger et al. Cadaveric tissue models have been used in laparoscopic cholecystectomy, endoscopic retrograde cholangiopancreatography and bronchoscopy training (Palter & Grantcharov, 2010). The advantages of these models include the ease of procurement, good tissue handling properties when fresh and a relatively low price (Munz et al. The disadvantages include anatomic differences from human anatomy, risk of infection, inherent costs of maintaining appropriate facilities with trained personnel, difficulties with procurement, as well as ethical considerations in using cadaver models for surgery training. Live anesthetized animal models are still being used in some countries for surgical skills training. Advantages of live animal models include high fidelity and realism of tissues, excellent tissue compliance, opportunities to simulate intra-operative complications and practice operations in their entirety, as well as the ability to induce bleeding for vascular procedures (Munz et al. The disadvantages include inability to use live anesthetized animals for 8 surgery training in some countries such as the United Kingdom, high acquisition and maintenance costs, ethical concerns about practicing on live animals, and differences from human anatomy (Munz et al. Does every task require a high fidelity simulator or can certain tasks be taught using low fidelity and low cost simulators? The answers to some of these questions are already available; others will require further scientific inquiry. Outcome metrics included the total number of hand movements, total distance traveled for each hand, total time taken to perform the task and the economy of movement. Technical skill was assessed on a synthetic Nissen fundoplication model and intra-operatively using a validated procedure-specific scale and a global rating scale. The annual cost of training 5 residents on the box trainer was reported as $11,975. A recent systematic review and meta-analysis of clinical trials up to May 11, 2011 compared simulation-based training in laparoscopic surgery to no intervention, to a non-simulation intervention and to a different simulation-based intervention (Zendejas, Brydges, Hamstra, & Cook, 2013). The outcomes of interest were: participants satisfaction, skill (in a test setting), and behavior when caring for patients. The pooled effect size favored the box trainer for the outcomes of participants satisfaction (effect 11 size 0. Two studies compared box trainers and animal models; two other studies compared box trainers and human cadaver models. In all four of these studies, the box trainer was favored for the outcome of skill (effect size 0. Based on the results of this systematic review, box trainers seem to be at least equivalent, if not superior, to other simulated training modalities when evaluated for the variables of participants satisfaction, skill, and behavior when caring for patients. This study did not, however, address the cost-effectiveness of different simulation modalities. Anders Ericsson has stated that expertise should not be ascribed to individuals with greatest experience, greatest accumulated knowledge or greatest number of peer nominations; rather, it should be ascribed to those individuals who demonstrate reproducibly superior performance (Ericsson, 2008). Applying this statement to the domain of surgery suggests that expert surgeons are those individuals that have reproducibly superior patient outcomes, rather than those surgeons that have performed the greatest number of operations. Deliberate practice is required and has been uniformly associated with improved performance in sports, music and medicine (Ericsson, 2004). According to Ericsson, four conditions are required for deliberate practice: (1) provision of a task with a well-defined goal; (2) motivation of an individual to improve; (3) provision of feedback; and (4) provision of ample opportunities for repetition and gradual refinement of performance. For a novice learner to learn a technical skill, the instructional process must begin by decomposing the task into context-free features and providing the rules for determining actions on the basis of these features. A useful illustrative example of this instructional process can be made for a medical student who is learning how to suture. The task of suturing can be decomposed into context-free rules of loading the needle, pronation of the wrist, entering tissue at 90 degrees, supination of the wrist and reloading the needle. These context-free rules are then taught to a medical student at the novice stage of skill acquisition. As the medical student gains increasing experience with real situations, he or she will learn to recognize aspects of these situations and will modify prior context-free rules according to these newly acquired aspects. With increasing situational experience, a novice medical student on a surgery rotation will build on the context-free rules of suturing by learning which type of suture and what type of stitch is useful in which situation.
Revision of Roux-En-Y gastric bypass for weight regain: a systematic review of techniques and outcomes symptoms dengue fever cheap 25 mg antivert with mastercard. Endobarrier in grade I obese patients with long-standing type 2 diabetes: role of gastrointestinal hormones in glucose metabolism medicine lodge ks order generic antivert pills. Comparison of safety and effectiveness between laparoscopic mini-gastric bypass and laparoscopic sleeve gastrectomy: A meta-analysis and systematic review treatment kidney failure buy 25 mg antivert with visa. Impact of initial response of laparoscopic adjustable gastric banding on outcomes of revisional laparoscopic Roux-en-Y gastric bypass for morbid obesity treatment diarrhea cheap 25 mg antivert otc. Bariatric Surgery Page 59 of 60 UnitedHealthcare Commercial Medical Policy Effective 12/01/2019 Proprietary Information of UnitedHealthcare medicine 5513 purchase 25mg antivert overnight delivery. When deciding coverage medicine abuse purchase 25 mg antivert otc, the member specific benefit plan document must be referenced as the terms of the member specific benefit plan may differ from the standard plan. Before using this policy, please check the member specific benefit plan document and any applicable federal or state mandates. UnitedHealthcare reserves the right to modify its Policies and Guidelines as necessary. This Medical Policy may also be applied to Medicare Advantage plans in certain instances. UnitedHealthcare Medical Policies are intended to be used in connection with the independent professional medical judgment of a qualified health care provider and do not constitute the practice of medicine or medical advice. Bariatric Surgery Page 60 of 60 UnitedHealthcare Commercial Medical Policy Effective 12/01/2019 Proprietary Information of UnitedHealthcare. The proven efficacy coupled with major reductions in perioperative morbidity and mortality has contributed to the widespread acceptance in the adult population, as well as an increasing acceptance in select pediatric and geriatric populations. Any practicing acute care surgeon can expect to increasingly encounter the post bariatric surgery patient who requires urgent evaluation and potentially surgical intervention. Therefore, a basic understanding of the common bariatric surgical procedures being performed and their associated short and long-term complication profiles is necessary to safely and effectively evaluate, triage, and manage these patients. If a bariatric surgeon is not immediately available at your center to assist or advise, then a telephone conversation with a bariatric specialist at a local referral center can be invaluable in providing advice and determining the necessity for transfer. This syllabus will provide a review of the most important bariatric-specific problems that may present to an acute care surgeon. There is nothing unique about abdominal emergencies in the bariatric patient versus other patients who have undergone prior foregut surgery, but there are specific additional considerations and triggers for interventions that the acute care surgeon should be aware of. Establish exactly what procedure the patient had done (many times they will all be lumped as having a prior gastric bypass), when and where it was done, open vs laparoscopic, and were there any immediate postoperative complications or problems. If possible, contacting the original bariatric surgeon can provide critical information or advice. In the early postop period (1-4 weeks) any patient presenting with significant abdominal complaints should be assumed to have a leak (anastomotic or staple line) until proven otherwise. Many abdominal emergencies present with associated pulmonary symptoms, and pulmonary embolism can present similar to a leak. Postoperative bowel obstructions after a gastric bypass are due to an internal hernia until proven otherwise. This proof usually requires surgical exploration done in a timely fashion to avoid catastrophic small bowel strangulation/necrosis or blowout of a proximal staple line. The sleeve gastrectomy is the fastest growing bariatric procedure now being performed, so be familiar with the anatomy and the common emergencies with this procedure. Although touted as a safer and less invasive option than gastric bypass, the leak rate is similar (or higher). Many acute abdominal complaints with the adjustable gastric band can be relieved by complete band deflation (can be done at bedside), turning an urgent issue into an elective one. They also should be given a decreased volume of oral contrast and do not require a full oral prep O Radiologists not familiar with bariatric imaging may have problems sorting out the anatomy. Face to face discussion and review of the studies is critical O A common mistake in evaluating the patient in the early postoperative period is interpreting concerning imaging findings as normal postop variants. Most early complications of laparoscopic gastric bypass can be managed laparoscopically in experienced hands, but do not hesitate to convert to open as needed. The most important concept to understand in the gastric bypass patient is the difference in the management of postop small bowel obstruction. If the roux limb was routed through a retrocolic defect, then herniation at this site is possible also. Progressive intolerance to solids > liquids and pain with eating are the usual presenting signs. Upper endoscopy should be performed and most strictures respond to serial balloon or bougie dilation. This is typically only seen after gastric bypass and not with other bariatric procedures. The incidence is 2-15% and varies by anastomotic techniques and patient populations. Common symptoms are epigastric pain with eating, but they can also present as spontaneous perforations. They can occur anywhere along the sleeve staple line, but are almost always at the proximal end (Figure). Endoscopic stenting to achieve adequate coverage of the leak is much more difficult compared to gastric bypass leaks, and should be referred to a very experienced endoscopic surgeon or gastroenterologist. If intraluminal bleeding forms a large hematoma it can cause obstruction and result in a proximal blowout leak as described above. Urgent endoscopy or surgical re-exploration should be performed to evacuate the hematoma. This is the angle formed by a straight line through the long axis of the band and a vertical line through the spinal column. Normal position is approximately 45 degrees (as shown in Figure), and anything > 58 degrees indicates slippage. This can also allow the band to slip back into normal position, but should still be followed by band removal or revision. An endoscopic strategy for management of anastomotic complications from bariatric surgery: a prospective study. Acute complications after laparoscopic bariatric procedures: update for the general surgeon. Diagnosis and management of acute and early complications of/after bariatric surgery. Imaging in bariatric surgery: a guide to postsurgical anatomy and common complications. American Society for Metabolic and Bariatric Surgery position statement on emergency care of patients with complications related to bariatric surgery. Bariatric surgery: a review of the available procedures and complications for the emergency physician. Use of endoscopic stents to treat anastomotic complications after bariatric surgery. Bariatric gastrectomy has become one of the most com surgery can effectively treat obesity and also monly performed bariatric operations. It is es improve or even resolve a number of related co sentially a restrictive bariatric operation; how morbidities, offering patients a better life. Articles on sleeve gastrec there is still a lack of standardization regarding the surgical technique. Standardizing the surgi tomy, published on Pubmed, Medline and Google cal technique is essential in order to minimize Scholar databases in English were thoroughly postoperative complications and offer patients revised and included in the discussion. It is relatively easy to perform, well tol erated by the patients and very effective regard ing long-term excessive weight loss and reso Sleeve gastrectomy was frst performed by lution of the comorbidities, with minimum nutri Hess in 1988 as part of his biliopancreatic diver tional defciencies. By removing the gastric fundus, patients undergoing sleeve It is well documented that obese patients are gastrectomy have markedly decreased levels of generally malnourished, mainly due to a non-var ghrelin and suppressed appetite respectively13. Vitamin D defciency is common dure, it is also an effective surgical technique, among obese patients due to malnutrition and limited sun exposure. Vitamin B12 is absorbed in the terminal ileum when banded to intrinsic factor, which is produced from the pari etal cells in the antrum and duodenum. Karamanakos Improvement in metabolic changes faction postoperatively and a signifcant number (diabetes) of them change their eating habits to a healthier diet over time56. Weiner et al50 reported that surgical techniques like single access surgery or hypertension either improved or resolved in 97% robotic surgery, with comparable results62-65. The of the patients, whereas dyslipidemia improved preoperative management of the patients under in 77% of the cases. Obstructive risk assessment and evaluation to exclude other sleep apnea, commonly seen in morbidly obese causes of obesity should be performed in every patients, can also be improved in 80% of patients patient. The agree that it is important to mobilize the fundus majority of patients report high rates of satis before transection and to resect the short gastric 4932 Sleeve gastrectomy, a review the last staple fring61. Soricelli et al73 tried to ex plain the vascular anatomy of this area, because one of the best supported theories of proximal fstula formation is the vascular-ischemic theo ry72. A critical area of vascularization is created at the angle of His and the resection on that area could lead to an ischemic gastric remnant, with an increased likelihood for a leak. Therefore, it is important to avoid resection too close to the esophagus and avoid creating a stenosis at the level of the angular incisure71. In order to maintain a standardized gastric vol ume and allow the reproducibility of the technique between different bariatric surgical teams a bougie is used during the gastric division to facilitate the resection. However, the size of the bougie is not standard and various sizes have been used from Figure 2. The bougie size is different bougie sizes and different starting and ending tran measured in French (Fr) where 1 Fr equals 0. Most surgeons use a bougie between 32-40 Fr and, considering the vessels before stomach division. This will assist above, we can safely assume that they practically the creation of a small gastric pouch and allow use the same bougie size61,74. If a hiatal have been associated with a higher incidence of hernia is present, it should be repaired at the same staple line leaks, longer hospital stay, tendency time by posterior crural approximation19. Using bigger the distance from the pylorus at which the gastric than 40 Fr bougies, reduces the relative risk for division should begin. As a matter of fact, bigger to perform a restrictive bariatric operation, with bougies result in larger gastric pouches and this improved gastric emptying and decreased intralu may affect the long-term weight loss. However, the line, although many authors do not routinely per bariatric surgeon should always consider the fact form this reinforcement61, 79. Another reason for that a smaller gastric pouch with intact gastric reinforcing the staple line is the control of postop antrum, leads to increased intraluminal pressures erative leaks. Fistulas on the staple line may be of and gastric emptying diffculties, that could place mechanical-tissular cause, when the intraluminal patients at higher risk for leaks and proximal fs pressure exceeds the staple line strength, or of tula formation at the gastroesophageal junction71. It seems that the ffth or sixth postoperative day, during the most experts agree on the importance to stay infammatory-proliferation phase of wound heal away from the gastroesophageal junction during ing. Karamanakos sular, leaks present early on the frst two postop tients, before a prospective second-stage bariatric erative days80. A number of different reinforcing materials prehensive interdisciplinary assessment by a team have been introduced and many studies have tried of specialists experienced in obesity manage to provide evidence for their use81-84. Sleeve gastrectomy line invagination with a simple running sero-se candidates should undergo routine preoperative rous suture, with or without the addition of an assessment, like any other major abdominal sur omental patch, could effciently control bleeding gery. How tions, it does not signifcantly reduce bleeding ever, super obese patients tend to regain weight complications and cannot be recommended as a after the frst 12 months of follow-up, while main standard technique61,86. Nevertheless, a negative test does not safe procedure for high-risk surgical patients. It exclude a postoperative leak and many authors can be used as a safe frst surgical procedure in do not perform these tests at all88,89. A simpler order to achieve rapid weight loss in high-risk pa test to discover a potential staple line defect is tients who need to undergo a second non-bariatric to infate the resected stomach with air using a procedure such as knee replacement, nephrec regular syringe89. Therefore, these patients 0% to 18%, with a 30-day postoperative mortality should be managed in bariatric centers of excel ranging from 0%-0. The postoperative lence that offer all available surgical options and a complications can be distinguished in early and strict long-term follow-up112. Morbid obesity in elderly patients is a substan Early complications generally involve bleed tial health problem. Perioperative management ing, gastric leak, obstruction, abscess formation, of medical complications is crucial. Usually, it occurs during Other indications may include cases that the the frst or second postoperative day and general small bowel is inaccessible due to adhesions from ly originates from the stapling line or the divided prior operations and patients in whom repeated gastroepiploic vessels. Chiu et al117 in their fusion and patient resuscitation, but there are systematic review concluded that there is not cases for which reoperation is necessary for the enough evidence to consolidate to a consensus defnite control of the bleeding119. Refux symptoms is that a leak happens when the intralumi initially present in the frst postoperative year, nal pressure exceeds the staple line or tissular they gradually improve and reappear after the strength125. Endoscopic stenting should be handled carefully and devices like after percutaneous drainage of an abscess is a staples, electrocautery or other surgical equip valid treatment option for a proximal leak61,128,131. A number the endoscopic use of fbrin glues, plugs or clips of studies investigated the use of staple line has also been reported, although their effcacy reinforcing materials81-84. The surgeon should wait for that staple-line reinforcement may reduce the in at least 12 weeks with conservative therapy be cidence of postoperative leaks86,87. In the midpoint of the transection, and a second con case of a re-intervention, conversion to gastric tinuous suture from this point to the end, with bypass, Roux-en-Y, or total gastrectomy can be or without an omental patch may be adequate in performed61,132,133. Many authors routinely perform upper gas the intact pylorus, the removal of the antrum, trointestinal swallow studies postoperatively in the severely restricted gastric capacity and the order to evaluate the presence of an early leak, disrupted motility could create stasis and induce between the frst and third postoperative day. When the re However, the sensitivity of these studies is low section is not close enough to the esophagus, a and a negative test does not exclude the pres neofundus could form, which could also aggra ence of a leak126,128-130.
These hips tend to be stable in positions of extension medicine januvia discount 25mg antivert fast delivery, abduction medications removed by dialysis generic 25mg antivert otc, and external rotation medications 44334 white oblong purchase 25 mg antivert fast delivery. Most patients are instructed not to flex the hip greater than 90 degrees or adduct the leg across midline treatment for pink eye order antivert no prescription, especially during the? Patients are instructed not to sleep on the affected hip and to keep pillows between their knees to prevent adduction of the hip k-9 medications buy generic antivert 25 mg on-line. What are different types of surgical approaches used for hip arthroplasty and how do they impact rehabilitation? The most common approaches performed today are the anterolateral medicine ball workouts buy antivert 25 mg low cost, direct lateral, and posterior. The anterolateral approach is performed by developing an interval between the tensor fascia lata and gluteus medius with either partial reflection of the medius or takedown of the greater trochanter to expose the underlying hip joint. After the components are placed, the posterior capsule and conjoint tendon are repaired. The anterolateral approach has been shown to have a lower rate of postoperative hip dislocation, as the posterior hip soft tissues are not violated. However, with this approach time is needed to allow the gluteus medius repair or greater trochanter osteotomy to heal, often restricting active hip abduction and full weight-bearing. The posterior approach preserves the integrity of the gluteus medius and greater trochanter and allows wide exposure of the hip and proximal femur often needed for revision surgery. Implications for rehabilitation include avoidance of active hip abduction exercises following anterolateral and 539 540 the Hip and Pelvis direct lateral approaches for at least 6 weeks and more stringent adherence to total hip precautions following posterior hip approaches because of the potential for hip dislocation. Most patients will be able to achieve 110 to 120 degrees of hip flexion and will have the needed 160 degrees of combined hip flexion, abduction, and external rotation motion necessary to put on socks and shoes by 6 weeks after surgery. You notice that a patient you are treating following total hip arthroplasty has developed increased calf swelling and localized tenderness. There are several serious but relatively infrequent complications, including loosening/osteolysis, dislocation, periprosthetic fractures, sciatic nerve injury, heterotopic ossi? Dislocation following total hip arthroplasty is a multifactorial problem with reported rates ranging from 1% to 10%. The prevalence of dislocation has been related to posterior surgical approaches, smaller prosthetic femoral head size, surgical technique, revision surgery, and patient compliance. In a Mayo Clinic study of 19,680 hips, it was found that the incidence of dislocation was 1. The incidence of dislocation also increased after revision surgery to between 9% and 21%. The femoral nerve and the peroneal branch of the sciatic nerve are more likely to recover than injuries to the tibial branch or the entire sciatic nerve. Postoperative limp has been associated with takedown of the greater trochanter and hip abductor muscles. It has been found that the strength of the muscles surrounding Total Hip Arthroplasty 541 the operated hip joint was 84% to 89% of the strength of the uninvolved side in men, and 79% to 81% of the strength of the uninvolved hip in women. Physical therapy early in total hip arthroplasty does restore range of motion, but signi? In addition, the surgeons recommended that patients with hip revisions abstain from sexual activity for slightly longer time periods; because of the higher rate of reported instability, time is needed to allow for pericapsular and muscular healing. It was also recommended that extreme hip flexion, adduction, and internal rotation be avoided. Before surgery, all patients had severe pain and stiffness while playing; this was decreased to 31% of patients after 1 year, and only 16% reported having pain at the time of the survey (which was a mean of 8 years following surgery). In a study of 28 physicians surveyed at the Mayo Clinic, 3 physicians approved of total hip replacement patients returning to tennis; 9 physicians approved only doubles tennis. Most golfers returned within 3 to 4 months following surgery, while some returned at 4 weeks after surgery. Of hip society surgeons, 96% permitted or did not discourage golf after total hip arthroplasty, and 68. Subjects that exercised before total hip replacement demonstrated progress that was 3 months ahead of that seen in the control group during early rehabilitation. The exercise group had two 1-hour supervised exercise sessions and also performed home exercises 2 times a week. The exercise group demonstrated greater stride length and gait velocity at 3 weeks after surgery. What is the postoperative weight-bearing status of a total hip arthroplasty patient? Patients with cemented joint replacements can weight-bear as tolerated unless the operative procedure involved a soft tissue repair or internal? Patients with cementless or ingrowth joint replacements are put on partial weight-bearing or toe-touch weight-bearing for 6 weeks to allow maximum bony ingrowth to take place. What types of patients are candidates for minimally invasive total hip arthroplasty? Patients that qualify for a mini-invasive total hip replacement have a lower average body mass index, are thinner and healthier, and have fewer medical comorbidities. Mini-invasive hip replacements reduce blood loss, transfusion requirements, postoperative pain, and hospital stays. Dislocation rates have been found to be between 2% and 10%, and 35% of those patients do not have a reoccurrence. Three times more patients ambulate on day 1 and 50% more patients meet all discharge criteria by day 3 with minimally invasive total hip arthroplasty: discharge criteria were ability to transfer, ambulate with assistive device, and negotiate stairs independently. The average time for patients to discontinue the use of crutches was 6 days, 9 days to walk independently without an assistive device, 10 days to resume activities of daily living, and 16 days average time to walk 1? What are the pros and cons of the different types of arthroplasty surfaces: metal-on-metal, ceramic-on-ceramic, and metal-on-polyethylene? Metallosis and its effect on accelerating macrophage responses can damage the shell or femoral neck. There are elevated ion levels in the blood and urine, effects of which are unknown. There are also possible links to cancer because cobalt and chromium have been found to cause cancer in animals, but more research must be done on this. There is accelerated wear with higher degrees of abduction of the acetabular component. Ceramics are also high in cost and have increased rates of acetabular component loosening. Cross-linked polyethylene has been found to have better wear rates than standard polyethylene. Jackson-Trudelle E et al: Outcomes of total hip arthroplasty: a study of patients one year postsurgery, J Orthop Sports Phys Ther 32:260-267, 2002. Silva M et al: Metal-on-metal total hip replacement, Clin Orthop Relat Res 430:53-61, 2005. Warrick D: Death and thromboembolic disease after total hip replacement: a series of 1162 cases with no routine chemical prophylaxis, J Bone Joint Surg 77B:6-10, 1995. By the third or fourth month of fetal life, the membranes are resorbed, and the knee becomes a single chamber. The suprapatellar plica divides the suprapatellar pouch from the remainder of the knee. It lies on the medial wall of the joint, originating suprapatellarly and coursing obliquely down to insert on the infrapatellar fat pad. This wider and thicker plica is located along the lateral parapatellar synovium, inserting on the lateral patellar facet. The plica found to be the least symptomatic of all?the infrapatellar plica or ligamentum mucosum?is ironically the most commonly encountered plica. This bell-shaped remnant originates in the intercondylar notch, widens as it traverses the anterior joint space, and attaches to the infrapatellar fat pad. The capacity for this plica to block or obscure arthroscopic portal entry sites or interfere with visualization may be its only known signi? An irritated plica also may cause a pseudo-locking as the knee is extended and may pop beneath the patella or snap over the medial femoral condyle. Classic open kinetic chain or non?weight-bearing descriptions of patellofemoral tracking suggest that during the initial 20 degrees of knee flexion, there is no contact between the patella and femur. At 20 to 30 degrees of knee flexion, the distal third of the patella makes contact with the uppermost portion of the femoral condyles, with initial contact occurring between the lateral femoral condyle and the lateral patellar facet. At 45 degrees of knee flexion, the middle third of the patella contacts the femur. In summary, as flexion angle increases, 547 548 the Knee the contact area moves from proximal to distal on the femur and from distal to proximal on the patella. Additionally, femoral rotation creates increased patellofemoral contact pressures on the contralateral patellar facets, while tibial rotation creates increased patellofemoral contact pressures on the ipsilateral patellar facets. The meniscotibial portion of the capsule secures the menisci to the tibial plateau. Because the anterior lateral portion of the capsule, just lateral to the patella tendon, is quite thin, Hughston and others refer to it as the lateral blow-out?sign. Each step at heel strike with the knee near full extension exerts tremendous force across the posterior lateral knee. The arcuate complex (posterior one third of lateral supporting structures including the lateral collateral ligament, the arcuate ligament, and the extension of the popliteus) helps to control internal rotation of the femur on the? The posterior lateral bundle becomes more taut in extension, and the anterior medial bundle becomes more taut in flexion. Once past 30 degrees, the tendon slips behind the horizontal axis of the knee, providing force for flexion. It has attachments into the linea aspera, which are very strong and help to prevent the pivot-shift. A high Q-angle (intersection formed by lines drawn from the anterior superior iliac spine to the center of the patella and from the center of the patella to the tibial tuberosity; normally 13 degrees in males and 18 degrees in females) predisposes the patella to sublux laterally. With the addition of a loose retinaculum, patella alta, and a weak or dysplastic vastus medialis obliquus muscle, the 550 the Knee patella can easily sublux in the? With a flattened lateral femoral condyle, the patellofemoral joint becomes unstable, even though the patella is seated in the trochlear groove. If patella alta is present, the patella may not be in the groove, thus increasing stress on the patellar tendon. It is the thinnest articular cartilage layer and has the highest collagen content arranged at right angles to adjacent bundles and parallel to the articular surface. This layer has the greatest ability to resist shear stresses and serves to modulate the passage of large molecules between synovial fluid and articular cartilage. The design of this layer reflects the transition from the shearing forces of the super? It is known for vertical columns of cells that anchor the cartilage, distribute loads, and resist compression. The cruciate ligaments also twist upon themselves during knee flexion and extension. The weight-bearing line or mechanical axis of the femur on the tibia is normally biased slightly toward the medial side of the knee, creating a 170 to 175-degree angle between the longitudinal axis of the femur and tibia, which is opened laterally. If this alignment is altered by degenerative changes, fracture, or genetic conditions, excessive stress is placed on either the medial or the lateral tibiofemoral joint compartment. Tibial varum or femoral valgus (angle greater than 170 to 175 degrees) leads to increased medial compartment stress, whereas femoral varum or tibial valgus (angle less than 170 to 175 degrees) leads to increased lateral compartment stress. Are there differences between female and male knee joint anatomy and biomechanics? However, females tend to have a wider pelvis, greater femoral anteversion, more frequent evidence Functional Anatomy of the Knee 551 of a coxa varus?genu valgus hip and knee joint alignment with lateral tibial torsion, a greater Q angle (18 degrees versus 13 degrees), more elastic capsuloligamentous tissues, a narrower femoral notch, and smaller diameter cruciate ligaments. What is the normal amount of tibial torsion and how does the physical therapist measure it clinically? Tibial torsion can be measured by having the patient sit with their knees flexed to 90 degrees over the edge of an examining table. The therapist then places the thumb of one hand over the prominence of one malleolus and the index? Looking directly down over the end of the distal thigh, the therapist visualizes the axes of the knee and of the ankle. These lines are not normally parallel but instead form a 12 to 18-degree angle because of lateral tibial rotation. While both menisci are prone to injury, the medial meniscus is at greater injury risk for both isolated and combined injury in the young athlete because of its adherence to the medial collateral ligament. In addition to transverse plane rotatory knee joint loads, any direct blows to the lateral aspect of the knee while the foot is planted may lead to injury at both the medial collateral ligament and the medial meniscus. The lateral meniscus is more often injured in combination with noncontact anterior cruciate ligament injury. The popliteus musculotendinous complex functions as a kinesthetic monitor and controller of anterior-posterior lateral meniscus movement?for unlocking and internally rotating the knee joint during flexion initiation, and for balance or postural control during single-leg stance. Increased popliteus activity during tibial internal rotation with concomitant transverse plane femoral and tibial rotation lends support to the theory that it withdraws and protects the lateral meniscus, prevents forward dislocation of the femur on the tibia, and provides an equilibrium adjustment function. Popliteus activation may be most essential during movements performed in midrange knee flexion, when capsuloligamentous structures are unable to function optimally. The anatomic location, biomechanic function, muscle activation, and kinesthesia characteristics of the popliteus musculotendinous complex suggest that it warrants greater attention during the design and implementation of lower extremity injury prevention and functional rehabilitation programs. Nyland J et al: Anatomy, function, and rehabilitation of the popliteus musculotendinous complex, J Orthop Sports Phys Ther 35:165-179, 2005. The intersection of these two lines is the Q-angle; the normal value for this angle is 13 to 18 degrees. Because the Q-angle is a measure of bony alignment, it can be altered only through bony realignment surgical procedures. Yagi M et al: Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction, Am J Sports Med 30:660-666, 2002. Yasuda K et al: Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts, Arthroscopy 20:1015-1025, 2004. The Q-angle is measured by extending a line through the center of the patella to the anterior superior iliac spine and another line from the tibial tubercle through the center of the patella.
Dumping Syndrome and Hypoglycaemia: Dumping refers to the post-prandial occurrence of a constellation of symptoms elicited by the rapid transit of calorie-dense food to the small bowel treatment math definition proven 25 mg antivert. Dumping syndrome was believed to be typical of gastric bypass (70?75% of patients in the first year after surgery) [4] medications blood thinners purchase antivert 25 mg with mastercard, but it has been described also after sleeve gastrectomy (40% of patients 6 months after surgery) [15] treatment impetigo discount antivert 25 mg visa. Some authors suggested a possible role of dumping in determining weight loss after gastric bypass medicine lyrics antivert 25 mg sale, through the negative conditioning for consuming energy-dense foods [16] symptoms 24 hour flu cheap antivert 25mg, but this role has been questioned [17] medications identification order 25mg antivert otc. In clinical practice, symptoms of dumping syndrome can be classified as early or late, depending on how soon after food ingestion they occur: early symptoms occur about 10?30 min after meal, whereas late symptoms occur 1?3 h after food ingestion [20]. Late dumping is strictly related to the occurrence of reactive hypoglycaemia and may be more linked to changes in gastro-intestinal hormones and insulin secretion [21, 22]. Nutritional tips comprise eating small but frequent meals, avoiding ingestion of liquids within 30 min of a solid-food meal, avoiding simple sugars, increasing intake of fibre and complex carbohydrates and increasing protein intake [4]. List of graded clinical practical recommendations for post-bariatric micronutrients supplementation Recommendations Level of Grade of evidence recommendation* Long-term mineral and multivitamin supplementation should be 3 D prescribed to every bariatric patient according to the procedure. Periodic laboratory surveillance for nutritional deficiencies is recommended and supplementation should be individualized accordingly, with patients with demonstrated micronutrient deficiencies treated with the respective micronutrient. Oral or parenteral thiamine supplementation should be promptly 4 D started in every bariatric patient suffering from persistent vomiting severe enough to interfere with regular nutrition, even in the absence or before confirmatory laboratory data. Medical therapy has its role in patients who fail to be controlled with dietary modi fications. Several drugs have been described as beneficial in symptom control, but without consistent success. However, in case of severe hypoglycaemic events with neuroglycopenic symptoms, alternative causes of hyperinsulinaemic hypoglycaemia (pancreatic beta-cells hyperplasia, insulinoma) should be considered and specific diagnostic algorithms have been proposed [24]. Micronutrient Supplementation the occurrence of vitamin and mineral deficiencies is one of the most common and compelling problems after bariatric surgery. Prevention, detection and treatment of these deficiencies represent cornerstones of long-term follow-up in post-bariatric patients. In this section, first-level information about general and procedure-specific nutritional deficits, recommended micronutrient supplementation and nutritional follow-up is included. A short list of graded clinical practical recommendations on micronutrient supplementation is given in table 4. General and Procedure-Specific Nutritional Deficits the anatomical characteristics and the mechanisms of action of the various procedures mostly dictate the frequency and severity of vitamin and mineral deficiencies after bariatric surgery (table 5). Nutritional deficiencies are uncommon after purely gastric restrictive procedures not altering intestinal continuity and normal digestive processes, but more common after surgical procedures inducing some degree of malabsorption [4]. However, the occurrence of nutritional deficits is also influenced by factors independent from the surgical technique, such as regular and nutrient-dense food intake and adherence with post-operative vitamin and mineral supplementation. Detailed descriptions of vitamin and mineral deficiencies that may be encountered after bariatric surgery, their symptoms and consequences, and the rationale for vitamin supplementation have already been published [4?6, 25]. Iron: Iron deficiency with or without anaemia is common after gastric bypass, biliopan creatic diversion and duodenal switch [4], but it occurs also after sleeve gastrectomy [26] and more rarely after adjustable gastric banding [5, 25]. First, iron absorption occurs mostly in the duodenum and proximal jejunum, the gut sections that are bypassed in some procedures. Second, decreased acid production in the stomach and accelerated gastric emptying impair the reduction of iron from the ferric (Fe3+) to the absorbable ferrous state (Fe2+). Third, the intake of iron-rich foods (meats, enriched grains and vegetables) is frequently low. Finally the absorption of iron may be inhibited by inter action with other nutritional supplements (calcium) [4, 5]. Prophylactic empiric iron supple mentation is recommended after gastric bypass, biliopancreatic diversion, duodenal switch and sleeve gastrectomy [4, 5]. Iron is usually included in oral multivitamin and mineral prep arations with the inclusion of vitamin C, that is able to increase iron absorption [4] ; they should not be taken along together with calcium supplements. Cobalamin stores are usually high and vitamin B12 deficiency is therefore rare in the first year after surgery, but tends to increase with time [4]. Despite the absence of evidence-based recommendations, vitamin B12 supplementation is usually recommended after gastric bypass, sleeve gastrectomy, biliopancreatic diversion and duodenal switch [4]. Alternatively suggested regimens of administration are 1 mg/month intramuscularly, 3 mg every 6 months intramuscularly or 500? Folic Acid:Folate deficiency is uncommon after bariatric surgery because folate absorption occurs throughout the entire small bowel [4]. Anyway, folic acid is usually contained in the multivitamin and mineral supplements routinely used in bariatric patients. Calcium and Vitamin D: Calcium absorption occurs preferentially in the duodenum and proximal jejunum and is facilitated by vitamin D in an acid environment. Calcium absorption would therefore decrease after any bariatric procedure involving a bypass of the first intes tinal loops, reducing gastric acid production and lowering vitamin D levels. Vitamin D is a fat soluble vitamin absorbed preferentially in the jejunum and ileum. Therefore, a high incidence of vitamin D deficiency (50?60% of the patients) despite routine supplementation has been reported after biliopancreatic diversion [27, 28], gastric bypass [29] and omega-loop gastric bypass [30]. No significant decreases in vitamin D levels have been observed after sleeve gastrectomy [26] or adjustable gastric banding [31]. The most important consequence of coupled calcium and vitamin D deficiencies is bone demineralisation. Therefore, even in the absence of conclusive evidence concerning the long-term risk of fractures after bariatric surgery, calcium and vitamin D routine supplementation is strongly recommended after gastric bypass and malabsorptive procedures [4?6, 25]. Obese patients frequently present vitamin D deficiency at baseline; this deficiency should be corrected before surgery with an oral vitamin D load [5]. After surgery, the regular consumption of 1,200?2,000 mg/day of elemental calcium along with 400?800 U of vitamin D is recommended [4]. Calcium citrate should be preferred to calcium carbonate because it is better absorbed in the absence of gastric acid [5]. This standard supplementation is frequently insufficient to maintain suffi cient vitamin D levels in patients with malabsorption, and much higher oral or parenteral doses may be required. Therefore, the adequacy of calcium and vitamin D supplementation should be checked in any patients, with regular controls of markers of bone mineral metab olism. In post-bariatric patients with established osteoporosis pharmacologic treatment with bisphosphonates may be considered. Before starting bisphosphonate treatment, vitamin D deficiency needs to be fully corrected in order to avoid severe hypocalcaemia, hypophosphatemia, and osteomalacia [4]. Intra venous bisphosphonates are the preferred choice because of concerns about low absorption and potential risk of anastomotic ulcer with oral bisphosphonates [6]. Recommended intra venous drugs were zoledronate (5 mg once a year) or ibandronate (3 mg every 3 months), whereas oral bisphosphonates were alendronate (70 mg/week), risedronate (35 mg/week or 150 mg/month) and ibandronate (150 mg/month) [6]. The effectiveness of both intra venous and oral bisphosphonates in improving bone mineralisation has never been proved specifically in bariatric patients. Fat-Soluble Vitamins: the absorption of any fat-soluble vitamin (A, E, K, D) is reduced after bariatric procedures causing fat malabsorption and steatorrhoea (biliopancreatic diversion and duodenal switch). Vitamin E deficiency can lead to anaemia, ophthalmoplegia and peripheral neuropathy. Thiamine: the human body has a low storage capacity for the water-soluble vitamin thiamine (vitamin B1) and can become rapidly devoid without regular and sufficient intake. Therefore, a short period of persistent vomiting impairing regular food intake can precipitate thiamine deficiency [5, 25]. Symptomatic thiamine deficiency has been described after a few weeks of intractable vomiting after any bariatric procedure, usually as a consequence of mechanical problems such as stoma stenosis after gastric bypass [32], excessive band tightness or band slippage after gastric banding [33] and stomach oedema with impaired nutrition after sleeve gastrectomy [34]. Cases of thiamine deficiencies have been reported also after biliopancreatic diversion [35]. These neurologic symptoms are rapidly aggravating and may cause permanent neurologic deficits. Therefore, oral or parenteral thiamine supplementation (50?100 mg/day) should promptly be considered and started in every bariatric patient suffering from persistent vomiting severe enough to interfere with regular nutrition, even in the absence or before obtaining confirmatory laboratory data [4, 5]. In symptomatic patients, oral supplementation may be used only after 1?2 weeks of parenteral administration (100 mg/day) and continued until symptom resolution [4]. In case of severe malnutrition with the need for nutrition support, refeeding syndrome should be considered and fluid and electrolyte status should be monitored [36]. Other Micronutrients: Other minerals (zinc, copper, selenium, magnesium, potassium) and vitamin (B6) deficiencies have been described after bariatric surgeries [4, 5, 25]. Routine supplementation with multivitamins and minerals is usually sufficient to prevent clinical problems. If higher doses of single trace elements are needed, timing of administration of these micronutrients should be considered due to the possible interference between elements for intestinal absorption (zinc and iron in particular) [37, 38]. Routine supplementation with adequate amounts of fat-soluble vitamins should be added to this regimen after bilio pancreatic diversion or duodenal switch [4]. Routine supplementation does not ensure an absolute prevention of deficiencies over time, mainly because of individual variations in micronutrient absorption, nutritional require ments and compliance. Therefore, periodic laboratory routine surveillance for nutritional deficiencies is recommended, and supplementation should be individualised accordingly in patients with demonstrated micronutrient insufficiencies or deficiencies [6]. A reasonable scheme for minimal periodic nutritional surveillance after bariatric procedures is proposed intable 6[39]. Management of Co-Morbidities Bariatric surgery has profound effects on obesity-related co-morbidities. These effects are in general positive, but they can occur very rapidly, requiring prompt modifications and adjustments of medical therapy. Moreover, the status of co-morbidities and their evolution should be monitored both in the short and in the long term after surgery. A short list of graded clinical prac tical recommendations on management of co-morbidities after bariatric surgery is reported in table 7. Bariatric surgery has been shown to improve metabolic status and to reduce micro and macrovascular complications and cardiovascular deaths in patients with type 2 diabetes [1, 41?43]. On the other hand, poor pre-operative glucose control can lead to an increased risk of peri-operative complications [6], and some studies suggest that optimal glucose control prior to surgery may improve the chances of diabetes remission after surgery [44]. Moreover, higher post-operative glucose levels can lead to increased morbidity [45]. Therefore, good blood glucose control pre and post-bariatric surgery is highly recommended. In general, caution should be the guide in treatment, with close follow-up of glucose levels before and immediately after surgery, until eating habits and food intake stabilise. List of graded clinical practical recommendations for the management of major obesity-related comorbidities after bariatric surgery Recommendations Level of Grade of evidence recommendation* Type 2 diabetes Bariatric surgery has profound effects on diabetes and can lead to 1 A prompt modifications and adjustments of medical therapy. Metabolic control should be optimized in preparation for a bariatric 2 C procedure. In patients with long lasting diabetes, diabetes complications and poor glucose control, HbA1c levels <8% are considered acceptable. On the day of surgery, glucose levels should be targeted at <140 mg/dl 3 D and short acting insulin should be used according to a correction factor of one unit of insulin for every 40 mg/dl above the level of 140 mg/dl. Metformin can be reassumed from the 3rd day after surgery providing 3 D that renal function has been controlled at a dosage of 850 mg, 1?2 times daily. In the first 7?10 days after surgery, treatment should be directed 3 D toward fasting glucose values and patients should be instructed to test sugar at least twice a day fast in the morning (target values: 100-120 mg/dl) and during the day (less than 180 mg/dl 2 h after a meal). In the first 7?10 days after surgery, use of sulfonylureas and 3 D medications that increase the risk of hypoglycaemia should be avoided. For patients still requiring insulin during their post-operative hospital 3 D staying, basal insulin should be continued at discharge, with strict glucose monitoring and tapering of insulin units for avoidance of hypoglycaemia. In cases of complicated glucose control in the early post-operative 3 D phase, consultation with an endocrinologist should be considered. After the first early post-operative period, standard diabetes 4 D guidelines should be followed for the management of patients still requiring pharmacologic anti-diabetic treatment after bariatric surgery. Dyslipidaemia Lipid-lowering medications should not be stopped after surgery 4 D unless clearly indicated. Patients with dyslipidaemia and on lipid modifying medications should be have lipid profiles and cardiovascular risk status reassessed periodically. Hypertension In the first week after surgery, blood pressure tends to go down and 4 D should be monitored actively, with prompt adjustment of blood pressure medications to the new therapeutic needs. Avoidance of diuretics may be suggested in this phase for the high risk of dehydration. Continued surveillance of blood pressure is needed after surgery, 4 D because of the high risk of recurrence over time. Treatment of hypertension in the long-term should adhere to current general guidelines, possibly avoiding anti-hypertensive medications with a known unfavourable effect on body weight. In the patients in whom hypertension have resolved, continued surveillance should be guided by recommended screening guidelines for the specific age group. Pre-Operative Glucose Control: Ideally, metabolic control should be optimised in patients with obesity and type 2 diabetes in preparation for a bariatric procedure. In patients with long lasting diabetes, diabetes complications and poor glucose control, HbA1c levels < 8% are considered acceptable, but levels > 8% calls for clinical judgement regarding pre-operative medical treatment [6]. The continuation of the regular medications on the day before surgery with a reduction of basal insulin dosage to 0. A simple scheme for basal insulin prescription at discharge after bariatric surgery Basal insulin needs before discharge Dose of basal insulin prescribed at discharge 10 units or less of basal insulin the same dose should be continued at discharge 10?19 units of basal insulin 10 units should be continued at discharge 20?29 units of basal insulin 15 units should be continued at discharge 30?39 units of basal insulin 20 units should be continued at discharge 40?49 units of basal insulin 30 units should be continued at discharge 50 units or more of basal insulin 40 units should be continued at discharge surgery, glucose levels should be targeted at <140 mg/dl and short-acting insulin should be used according to a correction factor of one unit of insulin for every 40 mg/dl above the level of 140 mg/dl. From the day following the operation until discharge from the hospital, similar to the routine treatment for a hospitalised patient, target glucose values should be 140?180 mg/dl with basal insulin at a dose of 0. In cases of complicated glucose control, consultation of an endocrinologist should be considered. Early Post-Operative Management (7?10 Days after Surgery): During this period, patients are required to consume fluids, and the caloric intake is minimal. For this reason, treatment is directed predominantly toward fasting glucose values.
25mg antivert mastercard. What Is Vertigo & Why Do We Get It?.
References
- Connolly SJ, Ezekowitz MD, Yusuf S, et al., RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361(12):1139-51.
- Socransky SS, Haffajee AD, Cugini MA, et al. Microbial complexes in subgingival plaque. J Clin Periodontol 1998;25: 134.
- A plea to abandon asthma as a disease concept. Lancet 2006;368(9537):705.
- Donohue JP, Thornhill JA, Foster RS, et al: Clinical stage B non-seminomatous germ cell testis cancer: the Indiana University experience (1965-1989) using routine primary retroperitoneal lymph node dissection, Eur J Cancer 31A:1599n1604, 1995.
- Tomaselli GF, Backx PH, Marban E: Molecular basis of permeation in voltage-gated ion channels, Circ Res 72:491-496, 1993.
- Margolin K, Ernstoff MS, Hamid O, et al. Ipilimumab in patients with melanoma and brain metastases: an openlabel, phase 2 trial. Lancet Oncol 2012;13(5):459-465.