Brian S. Johnston, MD
- Department of Diagnostic Imaging
- David Grant USAF Medical Center
- Travis AFB, California
Instead gastritis diet ���������� buy doxazosin 2 mg with mastercard, the comorbid opioid use disorder is indicated in the 4th character of the opioid-induced disorder code (see the coding note for opioid intoxication chronic gastritis with focal intestinal metaplasia doxazosin 2 mg online, opioid withdrawal gastritis diet 1200 generic doxazosin 2 mg with mastercard, or a specific opioid-induced mental disorder) gastritis medicine cvs cheap doxazosin uk. Instead the comorbid sedative atrophic gastritis symptoms webmd buy discount doxazosin on line, hypnotic gastritis diet soy milk discount doxazosin generic, or anxiolytic use disorder is indicated in the 4th character of the sedative-, hypnotic-, or anxiolyticinduced disorder (see the coding note for sedative, hypnotic, or anxiolytic intoxication; sedative, hypnotic, or anxiolytic withdrawal; or specific sedative-, hypnotic-, or anxiolytic-induced mental disorder). For example, if there is comorbid sedative-, hypnotic-, or anxiolytic-induced depressive disorder and sedative, hypnotic, or anxiolytic use disorder, only the sedative-, hypnotic-, or anxiolytic-induced depressive disorder code is given with the 4th character indicating whether the comorbid sedative, hypnotic, or anxiolytic use disorder is mild, moderate, or severe: F13. For example, if there is comorbid amphetamine-type or other stimulant-induced depressive disorder and amphetamine-type or other stimulant use disorder, only the amphetamine-type or other stimulant-induced depressive disorder code is given, with the 4th character indicating whether the comorbid amphetamine-type or other stimulant use disorder is mild, moderate, or severe: F15. Instead, the comorbid tobacco use disorder is indicated in the 4th character of the tobacco-induced disorder code (see the coding note for tobacco withdrawal or tobacco-induced sleep disorder). For example, if there is comorbid tobacco-induced sleep disorder and tobacco use disorder, only the tobacco-induced sleep disorder code is given, with the 4th character indicating whether the comorbid tobacco use disorder is moderate or severe: F17,208 for moderate or severe tobacco use disorder with tobacco-induced sleep disorder. It is not permissible to code a comorbid mild tobacco use disorder with a tobacco-induced sleep disorder. This specifier applies only to major neurocognitive disorders (including probable and possible). Note: As indicated for each subtype, an additional medical code is needed for probable major neurocognitive disorders, including those due to probable and possible medical etiologies. The medical etiology should be coded first, before the code for the major neurocognitive disorder. An additional medical code should not be used for possible major neurocognitive disorder or mild neurocognitive disorder. Major or Mild Coding note: For probable major neurocognitive disorder due to probable Frontotemporal frontotemporal lobar degeneration, with behavioral disturbance, code first G31. For probable major neurocognitive disorder due to probable frontotemporal lobar degeneration, without behavioral disturbance, code first G31. For possible major neurocognitive disorder due to possible frontotemporal lobar degeneration, with behavioral disturbance, code first G31. For major neurocognitive disorder due to possible frontotemporal lobar degeneration, without behavioral disturbance, code first G31. For probable Lewy Bodies major neurocognitive disorder with probable Lewy bodies, without behavioral disturbance, code first G31. For possible major neurocognitive disorder with possible Lewy bodies, with behavioral disturbance, code first G31. For possible major neurocognitive disorder with possible Lewy bodies, without behavioral disturbance, code first G31. Major or Mild Coding note: For probable major vascular neurocognitive disorder probably due to Vascular vascular disease, with behavioral disturbance, code F01. For probable major vascular Neurocognitive neurocognitive disorder probably due to vascular disease, without behavioral disturbance, Disorder code F01. For possible major vascular neurocognitive disorder possibly due to vascular disease, with or without behavioral disturbance, code G31. For major neurocognitive disorder possibly due to vascular disease, without behavioral disturbance, code F01. This prohibition apphes to unauthorized uses or reproductions in any form, including electronic applications. Countis, Field Operations Practice Research Network Manager, Practice Research Network Amy Porfiri, M. For some disorders, the code can be indicated only according to the subtype or specifier. Following chapter titles and disorder names, page numbers for the corresponding text or criteria are included in parentheses. Requiring support Specify if: With or without accompanying intellectual impairment. With onset during withdrawal Psychotic Disorder Due to Another Medical Condition^ (115) Specify whether: 293. In full remission Specify severity if full criteria for a mood episode are not currently met: Mild, Moderate, Severe 301. Specify current severity Sleep-Related Hypoventilation (387) Specify whether: 327. Specify whether: Substance intoxication delirium^ Substance withdrawal delirium^ 292. Note: As indicated for each subtype, an additional medical code is needed for probable major neurocognitive disorder or major neurocognitive disorder. With successive editions over the past 60 years, it has become a standard reference for clinical practice in the mental health field. It is a tool for clinicians, an essential educational resource for students and practitioners, and a reference for researchers in the field. Finally, the criteria and corresponding text serve as a textbook for students early in their profession who need a structured way to understand and diagnose mental disorders as well as for seasoned professionals encountering rare disorders for the first time. Also, within the text, subheadings on development and course provide descriptions of how disorder presentations may change across the lifespan. For added emphasis, these age-related factors have been added to the criteria themselves where applicable. Likewise, gender and cultural issues have been integrated into the disorders where applicable. The revised chapter structure was informed by recent research in neuroscience and by emerging genetic linkages between diagnostic groups. A more dimensional profile of personality trait expression is also proposed for a trait-specified approach. Additional cross-cutting and diagnostic severity measures are available online ( These innovations were designed by the leading authorities on mental disorders in the world and were implemented on the basis of their expert review, public commentary, and independent peer review. In addition, we are grateful to those who contributed so much time to the independent review of the revision proposals, including Kenneth S. One important aspect of this transition derives from the broad recognition that a too-rigid categorical system does not capture clinical experience or important scientific observations. Such an approach should permit a more accurate description of patient presentations and increase the validity of a diagnosis. In short, we have come to recognize that the boundaries between disorders are more porous than originally perceived.
Bereavement-related depression tends to occur in persons with other vulnerabilities to depressive disorders high fiber diet gastritis cheap doxazosin 2 mg mastercard, and recovery may be facilitated by antidepressant treatment gastritis all fruit diet cheap 2mg doxazosin mastercard. A more chronic form of depression gastritis diet ������ buy 1 mg doxazosin overnight delivery, persistent depressive disorder (dysthymia) gastritis symptoms lightheadedness discount doxazosin 4mg amex, can be diagnosed when the mood disturbance continues for at least 2 years in adults or 1 year in children gastritis diet coconut water cheap doxazosin 2mg on-line. Almost 20 years of additional of research on this condition has confirmed a specific and treatment-responsive form of depressive disorder that begins sometime following ovulation and remits within a few days of menses and has a marked impact on functioning gastritis mind map order doxazosin australia. A large number of substances of abuse, some prescribed medications, and several medical conditions can be associated with depression-like phenomena. The mood between temper outbursts is persistently irritable or angry most of the day, nearly every day, and is observable by others. The diagnosis should not be made for the first time before age 6 years or after age 18 years. There has never been a distinct period lasting more than 1 day during which the full symptom criteria, except duration, for a manic or hypomanie episode have been met. Individuals whose symptoms meet criteria for both disruptive mood dysregulation disorder and oppositional defiant disorder should only be given the diagnosis of disruptive mood dysregulation disorder. Diagnostic Features the core feature of disruptive mood dysregulation disorder is chronic, severe persistent irritabihty. This severe irritability has two prominent clinical manifestations, the first of which is frequent temper outbursts. The second manifestation of severe irritability consists of chronic, persistently irritable or angry mood that is present between the severe temper outbursts. However, rates are expected to be higher in males and school-age children than in females and adolescents. Development and Course the onset of disruptive mood dysregulation disorder must be before age 10 years, and the diagnosis should not be applied to children with a developmental age of less than 6 years. Because the symptoms of disruptive mood dysregulation disorder are likely to change as children mature, use of the diagnosis should be restricted to age groups similar to those in which validity has been established (7-18 years). Approximately half of children with severe, chronic irritability will have a presentation that continues to meet criteria for the condition 1 year later. Rates of conversion from severe, nonepisodic irritability to bipolar disorder are very low. Age-related variations also differentiate classic bipolar disorder and disruptive mood dysregulation disorder. Disruptive mood dysregulation disorder is more common than bipolar disorder prior to adolescence, and symptoms of the condition generally become less common as children transition into adulthood. In such children, a relatively extensive history of chronic irritability is common, typically manifesting before full criteria for the syndrome are met. However, these two groups do not differ in familial rates of anxiety disorders, unipolar depressive disorders, or substance abuse. For example, face-emotion labeling deficits, as well as perturbed decision making and cognitive control, are present in children with bipolar disorder and chronically irritable children, as well as in children with some other psychiatric conditions. Gender-Related Diagnostic issues Children presenting to clinics with features of disruptive mood dysregulation disorder are predominantly male. Because of their extremely low frustration tolerance, such children generally have difficulty succeeding in school; they are often unable to participate in the activities typically enjoyed by healthy children; their family life is severely disrupted by their outbursts and irritability; and they have trouble initiating or sustaining friendships. Levels of dysfunction in children with bipolar disorder and disruptive mood dysregulation disorder are generally comparable. Both conditions cause severe disruption in the lives of the affected individual and their families. In both disruptive mood dysregulation disorder and pediatric bipolar disorder, dangerous behavior, suicidal ideation or suicide attempts, severe aggression, and psychiatric hospitalization are common. In addition, during a manic episode, the change in mood must be accompanied by the onset, or worsening, of associated cognitive, behavioral, and physical symptoms. Thus, while bipolar disorders are episodic conditions, disruptive mood dysregulation disorder is not. In fact, the diagnosis of disruptive mood dysregulation disorder cannot be assigned to a child who has ever experienced a fuU-duration hypomanie or manic episode (irritable or euphoric) or who has ever had a manic or hypomanie episode lasting more than 1 day. Another central differentiating feature between bipolar disorders and disruptive mood dysregulation disorder is the presence of elevated or expansive mood and grandiosity. These symptoms are common features of mania but are not characteristic of disruptive mood dysregulation disorder. In addition, the diagnosis of disruptive mood dysregulation disorder requires severe impairment in at least one setting. That is, in only approximately 15% of individuals with oppositional defiant disorder would criteria for disruptive mood dysregulation disorder be met. Moreover, even for children in whom criteria for both disorders are met, only the diagnosis of disruptive mood dysregulation disorder should be made. Nevertheless, it also should be noted that disruptive mood dysregulation disorder appears to carry a high risk for behavioral problems as well as mood problems. Attention-deficit/hyperactivity disorder, major depressive disorder, anxiety disorders, and autism spectrum disorder. In addition, children with autism spectrum disorders frequently present with temper outbursts when, for example, their routines are disturbed. In that instance, the temper outbursts would be considered secondary to the autism spectrum disorder, and the child should not receive the diagnosis of disruptive mood dysregulation disorder. Children with symptoms suggestive of intermittent explosive disorder present with instances of severe temper outbursts, much like children with disruptive mood dysregulation disorder. Comorbidity Rates of comorbidity in disruptive mood dysregulation disorder are extremely high. It is rare to find individuals whose symptoms meet criteria for disruptive mood dysregulation disorder alone. Not only is the overall rate of comorbidity high in disruptive mood dysregulation disorder, but also the range of comorbid illnesses appears particularly diverse. These children typically present to the clinic with a wide range of disruptive behavior, mood, anxiety, and even autism spectrum symptoms and diagnoses. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning: at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure. Note: Do not include symptoms that are clearly attributable to another medical condition. Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down). The episode is not attributable to the physiological effects of a substance or to another medical condition. The dysphoria in grief is likely to decrease in intensity over days to weeks and occurs in waves, the so-called pangs of grief. Coding and Recording Procedures the diagnostic code for major depressive disorder is based on whether this is a single or recurrent episode, current severity, presence of psychotic features, and remission status. Current severity and psychotic features are only indicated if full criteria are currently met for a major depressive episode. Remission specifiers are only indicated if the full criteria are not currently met for a major depressive episode. Codes are as follows: Severity/course specifier Single episode Recurrent episode* Mild (p. In recording the name of a diagnosis, terms should be listed in the following order: major depressive disorder, single or recurrent episode, severity/psychotic/remission specifiers, followed by as many of the following specifiers without codes that apply to the current episode. Often insomnia or fatigue is the presenting complaint, and failure to probe for accompanying depressive symptoms will result in underdiagnosis.
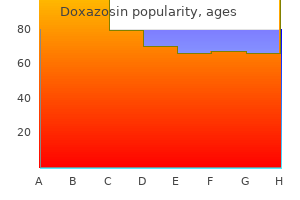
Because individuals with paranoid personality disorder lack trust in others diet makanan gastritis generic 2mg doxazosin visa, they have an excessive need to be self-sufficient and a strong sense of autonomy gastritis nunca mas purchase doxazosin. Because of their quickness to counterattack in response to the threats they perceive around them gastritis symptoms medscape doxazosin 1mg low price, they may be litigious and frequently become involved in legal disputes uremic gastritis symptoms generic doxazosin 2 mg amex. Individuals with this disorder seek to confirm their preconceived negative notions regarding people or situations they encounter gastritis diet emedicine cheap doxazosin 1mg visa, attributing malevolent motivations to others that are projections of their own fears gastritis drugs purchase doxazosin 1mg mastercard. They may exhibit thinly hidden, unrealistic grandiose fantasies, are often attuned to issues of power and rank, and tend to develop negative stereotypes of others, particularly those from population groups distinct from their own. Attracted by simplistic formulations of the world, they are often wary of ambiguous situations. They may be perceived as "fanatics" and form tightly knit "cults" or groups with others who share their paranoid belief systems. Particularly in response to stress, individuals with this disorder may experience very brief psychotic episodes (lasting minutes to hours). In clinical samples, this disorder appears to be more commonly diagnosed in males. C ulture-Related Diagnostic Issues Some behaviors that are influenced by sociocultural contexts or specific life circumstances may be erroneously labeled paranoid and may even be reinforced by the process of clinical evaluation. Members of minority groups, immigrants, political and economic refugees, or individuals of different ethnic backgrounds may display guarded or defensive behaviors because of unfamiliarity. Paranoid personality disorder can be distinguished from delusional disorder, persecutory type; schizophrenia; and a bipolar or depressive disorder with psychotic features because these disorders are all characterized by a period of persistent psychotic symptoms. For an additional diagnosis of paranoid personality disorder to be given, the personality disorder must have been present before the onset of psychotic symptoms and must persist when the psychotic symptoms are in remission. Paranoid personality disorder must be distinguished from symptoms that may develop in association with persistent substance use. Other personality disorders may be confused with paranoid personality disorder because they have certain features in common. It is therefore important to distinguish among these disorders based on differences in their characteristic features. However, if an individual has personality features that meet criteria for one or more personality disorders in addition to paranoid personality disorder, all can be diagnosed. Individuals with behaviors that meet criteria for schizoid personality disorder are often perceived as strange, eccentric, cold, and aloof, but they do not usually have prominent paranoid ideation. The tendency of individuals with paranoid personality disorder to react to minor stimuli with anger is also seen in borderline and histrionic personality disorders. Although antisocial behavior may be present in some individuals with paranoid personality disorder, it is not usually motivated by a desire for personal gain or to exploit others as in antisocial personality disorder, but rather is more often attributable to a desire for revenge. Individuals with narcissistic personality disorder may occasionally display suspiciousness, social withdrawal, or alienation, but this derives primarily from fears of having their imperfections or flaws revealed. A pervasive pattern of detachment from social relationships and a restricted range of expression of emotions in interpersonal settings, beginning by early adulthood and present in a variety of contexts, as indicated by four (or more) of the following: 1. Does not occur exclusively during the course of schizophrenia, a bipolar disorder or depressive disorder with psychotic features, another psychotic disorder, or autism spectrum disorder and is not attributable to the physiological effects of another medical condition. Individuals with schizoid personality disorder appear to lack a desire for intimacy, seem indifferent to opportunities to develop close relationships, and do not seem to derive much satisfaction from being part of a family or other social group (Criterion Al). They may have very little interest in having sexual experiences with another person (Criterion A3) and take pleasure in few, if any, activities (Criterion A4). These individuals have no close friends or confidants, except possibly a first-degree relative (Criterion A5). Individuals with schizoid personality disorder often seem indifferent to the approval or criticism of others and do not appear to be bothered by what others may think of them (Criterion A6). Associated Features Supporting Diagnosis Individuals with schizoid personality disorder may have particular difficulty expressing anger, even in response to direct provocation, which contributes to the impression that they lack emotion. Their lives sometimes seem directionless, and they may appear to "drift" in their goals. Such individuals often react passively to adverse circumstances and have difficulty responding appropriately to important life events. Because of their lack of social skills and lack of desire for sexual experiences, individuals with this disorder have few friendships, date infrequently, and often do not marry. Occupational functioning may be impaired, particularly if interpersonal involvement is required, but individuals with this disorder may do well when they work under conditions of social isolation. Data from the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions suggest a prevalence of 3. Development and Course Schizoid personality disorder may be first apparent in childhood and adolescence with solitariness, poor peer relationships, and underachievement in school, which mark these children or adolescents as different and make them subject to teasing. C ulture-Related Diagnostic issues Individuals from a variety of cultural backgrounds sometimes exhibit defensive behaviors and intefiersonal styles that may be erroneously labeled as "schizoid. Gender-Related Diagnostic issues Schizoid personality disorder is diagnosed slightly more often in males and may cause more impairment in them. To give an additional diagnosis of schizoid personality disorder, the personality disorder must have been present before the onset of psychotic symptoms and must persist when the psychotic symptoms are in remission. There may be great difficulty differentiating individuals with schizoid personality disorder from those with milder forms of autism spectrum disorder, which may be differentiated by more severely impaired social interaction and stereotyped behaviors and interests. Schizoid personality disorder must be distinguished from personality change due to another medical condition, in which the traits that emerge are attributable to the effects of another medical condition on the central nervous system. Schizoid personality disorder must also be distinguished from symptoms that may develop in association with persistent substance use. Although characteristics of social isolation and restricted affectivity are common to schizoid, schizotypal, and paranoid personality disorders, schizoid personality disorder can be distinguished from schizotypal personality disorder by the lack of cognitive and perceptual distortions and from paranoid personality disorder by the lack of suspiciousness and paranoid ideation. In contrast, people with schizoid personality disorder have a more pervasive detachment and limited desire for social intimacy. Individuals who are "loners" may display personality traits that might be considered schizoid. A pervasive pattern of social and interpersonal deficits marked by acute discomfort with, and reduced capacity for, close relationships as well as by cognitive or perceptual distortions and eccentricities of behavior, beginning by early adulthood and present in a variety of contexts, as indicated by five (or more) of the following: 1. Odd beliefs or magical thinking that influences behavior and is inconsistent with subcultural norms. Does not occur exclusively during the course of schizophrenia, a bipolar disorder or depressive disorder with psychotic features, another psychotic disorder, or autism spectrum disorder. Individuals with schizotypal personality disorder often have ideas of reference. These individuals may be superstitious or preoccupied with paranormal phenomena that are outside the norms of their subculture (Criterion A2). They may believe that they have magical control over others, which can be implemented directly. Individuals with this disorder are often suspicious and may have paranoid ideation. They are usually not able to negotiate the full range of affects and interpersonal cuing required for successful relationships and thus often appear to interact with others in an inappropriate, stiff, or constricted fashion (Criterion A6). Although they may express unhappiness about their lack of relationships, their behavior suggests a decreased desire for intimate contacts. They will interact with other individuals when they have to but prefer to keep to themselves because they feel that they are different and just do not "fit in. For example, when attending a dinner party, the individual with schizotypal personality disorder will not become more relaxed as time goes on, but rather may become increasingly tense and suspicious. Associated Features Supporting Diagnosis Individuals with schizotypal personality disorder often seek treatment for the associated symptoms of anxiety or depression rather than for the personality disorder features per se. In some cases, clinically significant psychotic symptoms may develop that meet criteria for brief psychotic disorder, schizophreniform disorder, delusional disorder, or schizophrenia. From 30% to 50% of individuals diagnosed with this disorder have a concurrent diagnosis of major depressive disorder when admitted to a clinical setting. Prevalence In community studies of schizotypal personality disorder, reported rates range from 0.
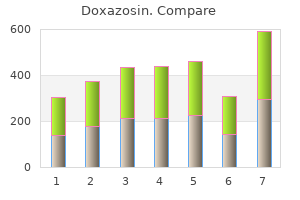
Specify current severity: Mild: Only one of the symptoms specified in Criterion B is fulfilled gastritis diet 4 rewards buy generic doxazosin on-line. Severe: Two or more of the symptoms specified in Criterion B are fulfilled prepyloric gastritis definition cheap 4 mg doxazosin with visa, plus there are multiple somatic complaints (or one very severe somatic symptom) gastritis diet for children buy doxazosin now. Somatic symptoms without an evident medical explanation are not sufficient to make this diagnosis gastritis garlic cheap doxazosin 4 mg free shipping. Individuals with somatic symptom disorder tend to have very high levels of worry about illness (Criterion B) gastritis flare up symptoms buy doxazosin us. They appraise their bodily symptoms as unduly threatening gastritis diet ocd purchase doxazosin 1mg free shipping, harmful, or troublesome and often think the worst about their health. In severe somatic symptom disorder, the impairment is marked, and when persistent, the disorder can lead to invalidism. Consequently, the patient may seek care from multiple doctors for the same symptoms. These individuals often seem unresponsive to medical interventions, and new interventions may only exacerbate the presenting symptoms. Associated Features Supporting Diagnosis Cognitive features include attention focused on somatic symptoms, attribution of normal bodily sensations to physical illness (possibly with catastrophic interpretations), worry about illness, and fear that any physical activity may damage the body. These behavioral features are most pronounced in severe, persistent somatic symptom disorder. These features are usually associated with frequent requests for medical help for different somatic symptoms. Any reassurance by the doctor that the symptoms are not indicative of serious physical illness tends to be short-lived and/or is experienced by the individuals as the doctor not taking their symptoms with due seriousness. The suggestion of referral to a mental health specialist may be met with surprise or even frank refusal by individuals with somatic symptom disorder. It is not known whether somatic symptom disorder is associated with suicide risk independent of its association with depressive disorders. The prevalence of somatic symptom disorder in the general adult population may be around 5%-7%. Females tend to report more somatic symptoms than do males, and the prevalence of somatic symptom disorder is consequently likely to be higher in females. Development and Course In older individuals, somatic symptoms and concurrent medical illnesses are common, and a focus on Criterion B is crucial for making the diagnosis. Somatic symptom disorder may be underdiagnosed in older adults either because certain somatic symptoms. Concurrent depressive disorder is common in older people who present with numerous somatic symptoms. It is the parent who may determine the interpretation of symptoms and the associated time off school and medical help seeking. Comorbid anxiety or depression is common and may exacerbate symptoms and impairment. Somatic symptom disorder is more frequent in individuals with few years of education and low socioeconomic status, and in those who have recently experienced stressful life events. C uiture-R eiated Diagnostic issues Somatic sjmnptoms are prominent in various "culture-bound syndromes. The relationship between number of somatic symptoms and illness worry is similar in different cultures, and marked illness worry is associated with impairment and greater treatment seeking across cultures. Despite these similarities, there are differences in somatic symptoms among cultures and ethnic groups. The description of somatic symptoms varies with linguistic and other local cultural factors. Seeking treatment for multiple somatic symptoms in general medical clinics is a worldwide phenomenon and occurs at similar rates among ethnic groups in the same country. Functional Consequences of Somatic Symptom Disorder the disorder is associated with marked impairment of health status. Many individuals with severe somatic symptom disorder are likely to have impaired health status scores more than 2 standard deviations below population norms. D ifferential Diagnosis If the somatic symptoms are consistent with another mental disorder. The presence of somatic symptoms of unclear etiology is not in itself sufficient to make the diagnosis of somatic symptom disorder. The symptoms of many individuals with disorders like irritable bowel syndrome or fibromyalgia would not satisfy the criterion necessary to diagnose somatic symptom disorder (Criterion B). Individuals with generalized anxiety disorder worry about multiple events, situations, or activities, only one of which may involve their health. The main focus is not usually somatic symptoms or fear of illness as it is in somatic symptom disorder. If the individual has extensive worries about health but no or minimal somatic symptoms, it may be more appropriate to consider illness anxiety disorder. The features listed under Criterion B of somatic symptom disorder may be helpful in differentiating the two disorders. In body dysmorphic disorder, the individual is excessively concerned about, and preoccupied by, a perceived defect in his or her physical features. In contrast, in somatic symptom disorder, the concern about somatic symptoms reflects fear of underlying illness, not of a defect in appearance. If another medical condition is present or there is a high risk for developing a medical condition. There is a high level of anxiety about health, and the individual is easily alarmed about personal health status. Illness preoccupation has been present for at least 6 months, but the specific illness that is feared may change over that period of time. Specify whether: Care-seeking type: Medical care, including physician visits or undergoing tests and procedures, is frequently used. Diagnostic Features Most individuals with hypochondriasis are now classified as having somatic symptom disorder; however, in a minority of cases, the diagnosis of illness anxiety disorder applies instead. Somatic symptoms are not present or, if present, are only mild in intensity (Criterion B). If a physical sign or symptom is present, it is often a normal physiological sensation. The preoccupation with the idea that one is sick is accompanied by substantial anxiety about health and disease (Criterion C). Individuals with illness anxiety disorder are easily alarmed about illness, such as by hearing about someone else falling ill or reading a healthrelated news story. This incessant worrying often becomes frustrating for others and may result in considerable strain within the family. Associated Features Supporting Diagnosis Because they believe they are medically ill, individuals with illness anxiety disorder are encountered far more frequently in medical than in mental health settings. The majority of individuals with illness anxiety disorder have extensive yet unsatisfactory medical care, though some may be too anxious to seek medical attention. They generally have elevated rates of medical utilization but do not utilize mental health services more than the general population. Individuals with the disorder are generally dissatisfied with their medical care and find it unhelpful, often feeling they are not being taken seriously by physicians. At times, these concerns may be justified, since physicians sometimes are dismissive or respond with frustration or hostility. This response can occasionally result in a failure to diagnose a medical condition that is present. The 1to 2-year prevalence of health anxiety and/or disease conviction in community surveys and population-based samples ranges fiOm 1. Deveiopment and Course the development and course of illness anxiety disorder are unclear. In older individuals, health-related anxiety often focuses on memory loss; the disorder is thought to be rare in children. Culture-Related Diagnostic issues the diagnosis should be made with caution in individuals whose ideas about disease are congruent with widely held, culturally sanctioned beliefs.
Discount doxazosin 2 mg otc. What causes yellow diarrhea after eating ? | Better Health Channel.
References
- Zerr DM, Gupta D, Huang M-L, et al. Effect of antivirals on human herpesvirus 6 replication in hemataopoietic stem cell transplant recipients. Clin Infect Dis. 2002;34:309-317.
- Gannon CJ, Zager JS, Chang GJ, et al. Pelvic exenteration affords safe and durable treatment for locally advanced rectal carcinoma. Ann Surg Oncol 2007;14:1870-77.
- Anderstrom CR, Fall M, Johansson SL: Scanning electron microscopic findings in interstitial cystitis, Br J Urol 63(3):270n275, 1989.
- Youngberg JA, Miller ED: Evaluation of percutaneous cannulations of the dorsalis pedis artery, Anesthesiology 44:80, 1976.
- Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med. 1993; 329(20):1463-6.
- Leijte JA, Kirrander P, Antonini N, et al: Recurrence patterns of squamous cell carcinoma of the penis: recommendations for follow-up based on a two centre analysis of 700 patients, Eur Urol 54(1):161n169, 2008.