Susan B Bressler, M.D.
- Professor of Ophthalmology

https://www.hopkinsmedicine.org/profiles/results/directory/profile/0000206/susan-bressler
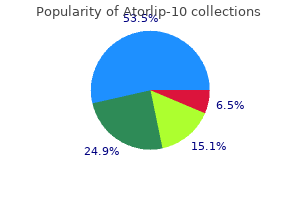
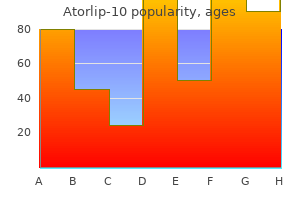
Similar arguments can support larynx-preserving surgery for glottic cancer although the guidelines all tend to recommend radiotherapy in preference to any form of surgery cholesterol ratio 4.2 atorlip-10 10 mg. Cordectomy in a small proportion of patients or vertical partial laryngectomy have both been proven to have similar local control to radiotherapy although their impact on voice quality have been shown to be worse than for radiotherapy (40) (41) cholesterol chart age buy generic atorlip-10 from india. There have been no randomised trials to compare outcomes between these different treatment modalities cholesterol test kit nz purchase atorlip-10 10mg otc. The British Columbia treatment guidelines suggest that locally advanced laryngeal cancer usually requires a combined approach although many patients may be curable with either modality alone and that multidisciplinary assessment is recommended cholesterol yahoo answers 10mg atorlip-10 free shipping. Larynx preservation with chemoradiotherapy (using laryngectomy for salvage) has been shown in randomised trials (42) (43) (44) (45) (46) (47) (48) (49) (50) to provide laryngeal preservation in the majority of cases without any detrimental effect on survival when compared with laryngectomy cholesterol test strips cardiochek order atorlip-10 paypal. Therefore cholesterol chart by age uk atorlip-10 10mg on line, it would be considered reasonable to offer radiotherapy to all patients with T3 laryngeal cancer and to reserve surgery for salvage. However, this is likely to be a small group and the majority of these will usually have locoregional symptoms requiring palliative radiotherapy. It may be possible in rare instances for a patient to have extensive M1 disease at diagnosis and not be recommended for radiotherapy. This would be a very small group and exclusion of these patients from the decision tree is unlikely to impact on the optimal radiotherapy utilisation estimate. Oropharynx There are no randomised trials addressing the treatment options (radiotherapy versus surgery) in oropharyngeal cancer. Therefore for the purposes of the decision tree, all oropharyngeal cancers are treated with radiotherapy. Radiation may be the preferred modality where the functional deficit will be great, and surgery may be the preferred modality where the functional deficit will be minimal. The results were identical in terms of relapse and survival between surgery and radiotherapy but the severe or fatal complication rate was substantially higher in the surgery group. The authors concluded that radiotherapy is the preferred primary treatment modality with surgical salvage reserved for persistent disease. Johns and Goldsmith (54) reviewed the literature and defined 4 groups of salivary gland tumours. The authors based their treatment of salivary gland malignancies on the size of the primary and the histopathologic diagnosis. Group 1 includes smaller tumours in the T1 and T2 classification with cell types that are associated with slow growth. T3 tumours and patients with nodal metastasis or recurrent tumours make up group 3. Radical parotidectomy with sacrifice of the facial nerve is usually required for a sufficient tumour-free margin in these patients, and postoperative radiotherapy is recommended. Group 4 includes T4 lesions and the extent of disease dictates excision and postoperative radiotherapy. Of all salivary gland tumours treated definitively, 81% were parotid, 18% submandibular, 1% sublingual. The remainder were high grade muco-epidermoid, adenocarcinoma, adenoid cystic, squamous cell carcinoma, malignant mixed or anaplastic tumours. Locoregional recurrence data for low-grade lesions treated with surgery alone were not reported. Local recurrence following surgery alone in the absence of adverse pathological features is reported by North et al. Surgical procedures included superficial (24%) or total (56%) parotidectomies and submandibular gland resection (20%). Since malignancy of the hypopharynx is generally clinically silent until the advanced stages, it is very unusual to diagnose these tumours at the T1 N0 stage. In addition, if the surgery of choice is pharyngolaryngectomy, then radiotherapy must be the preferred treatment to maintain function, using surgery for salvage. The proportion of these tumours that can be treated with conservative surgery alone would be so small as to make no significant difference to the overall utilisation rate. Therefore, all stages of hypopharynx cancer are recommended to have radiation for at least part of the treatment. The British Columbia group have not published guidelines for the management of paranasal sinus cancer. Accordingly in the decision tree, all non-metastatic nasopharyngeal carcinomas are designated to receive radiotherapy. The proportion of patients with M1 disease at diagnosis is small 5% in a series of 564 patients from Prince of Wales Hospital, Hong Kong (56), and 6% in 1555 patients with nasopharyngeal carcinoma treated at the National Taiwan University Hospital (57). A large proportion of these patients will however require radiotherapy for either locoregional symptoms or symptoms related to metastases to bone or brain. A small proportion of patients with liver and/or lung metastases will die from their disease without requiring radiotherapy. However, a detailed literature search failed to satisfactorily identify the proportion of patients that do not require radiotherapy. A study of all nasopharyngeal cancers treated in Finland 1980-1989 (58) revealed that 13/107 patients (12%) were treated palliatively due to age, severe co-morbidity or refusal to undergo radical radiotherapy. Metastatic squamous neck cancer with occult primary Indications for radiotherapy Most squamous carcinomas metastatic to lymph nodes of the upper half of the neck will originate from a head and neck primary site. However, in these patients the primary remains occult following standard head and neck examination and investigations. The indications for the use of radiotherapy either as definitive treatment or as an adjuvant to surgery for patients with metastatic squamous cell carcinoma of the head and neck where the primary is unidentified is controversial. The main intent is to not only maximise locoregional control in the neck but also to attempt to prevent the occult primary from becoming symptomatic. The Peter MacCallum Cancer Institute has developed treatment pathways for unknown primary squamous cell carcinoma of the head and neck (personal communication Prof. In their treatment pathway, routine radiotherapy either pre or post-operatively is recommended for >N2a disease and radiotherapy is considered optional for disease N1-2a. For the decision tree, the branch point for radiotherapy is for N1-2a not to receive radiotherapy. However, in the sensitivity analysis the branch point underwent modelling with the prevalence varying between the proportion with >N1 disease and > N2A disease receiving routine post operative radiotherapy to assess the impact that this variation has on the overall radiotherapy utilisation rate. From 1983-1992, 69 patients with unknown primary cancers of the head and neck were treated. All patients in this group maintained locoregional control (but the number of patients was very small). These data differs from that of Nguyen at al from the McGill University teaching hospital (36), who reported on 54 patients with metastatic squamous cell carcinoma to cervical lymph nodes. The decision tree uses the Sinnathamby rate of 9-22% of patients not receiving routine radiotherapy since this is the largest series and being Australian, this data is more likely to reflect incidence rates in other Australian treatment centres. The vast majority of N2a disease received radiation to the neck and head and neck mucosal sites. Recurrence or development of a symptomatic primary occurred in 54% of the N1-2 surgery alone group. None of the identified guidelines discuss the management of recurrent disease in this situation. However, it seems reasonable to assume that the vast majority of patients who develop recurrent disease would receive radiotherapy as part of their management, either alone for unresectable disease or post-operatively. Optimal Radiotherapy Utilisation Rate and Sensitivity Analysis Sensitivity analysis allows the assessment of the impact of varying the value of uncertain data items on the overall optimal radiotherapy utilisation rate. For the head and neck decision tree, 4 data items were identified as being uncertain. We therefore used incidence data to model between patients having radiotherapy for tumours > 4 cm in size as the smallest case scenario for radiotherapy (6% incidence) and >2 cm as the greatest case scenario for radiotherapy (25% incidence). To assess the impact of this uncertainty on the overall estimate of the need for radiotherapy in all head and neck cancers, a sensitivity analysis was performed for each of the variables. Once the decision trees for all tumours are completed, a tornado analysis will be performed whereby the impact of each of these variables on the overall estimate of the proportion of cancer patients needing radiotherapy will be examined. The graphs below show that the optimal proportion of head and neck cancer patients who should receive radiotherapy based on evidence is 78%. As head and neck cancer comprises 4% of all cancers, head and neck cancer patients suitable for radiotherapy represent 3. If early oral cancer were more routinely treated with radiotherapy then the utilisation rate would increase from 78% to 84%. This represents an increase in utilisation for head and neck cancer of 6% and an increase in the utilisation for all cancer by 0. Table 4: Optimal radiotherapy utilisation rates by head and neck sub type Tumour Sub-site % of head Overall optimal Proportion of all and neck radiotherapy cancer patients cancer utilisation rate that should for sub-site receive (%) radiotherapy (%) Oral Cavity 28 78 0. Prognostic factors for local recurrence, metastasis, and survival rates in squamous cell carcinoma of the skin, ear and lip. Carcinoma of the supraglottic larynx: treatment results with radiotherapy alone or with planned neck dissection. Carcinoma of the major salivary glands treated by surgery or surgery plus postoperative radiotherapy. Cervical lymph node metastases from unknown primary tumours Results from a national survey by the Danish Society for Head and Neck Oncology. Supracricoid partial laryngectomy with cricohyoidoepiglottopexy and cricohyoidopexy for glottic and supraglottic carcinomas. Treatment of early stage squamous cell carcinoma of the glottic larynx: endoscopic surgery or cricohyoidoepiglottopexy versus radiotherapy. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. Five-year update of a randomized trial of alternating radiotherapy and chemotherapy compared with radiotherapy alone in treatment of unresectable squamous cell carcinoma of the head and neck. Hyperfractionated radiation therapy with or without concurrent low-dose daily cisplatin in locally advanced squamous cell carcinoma of the head and neck: a prospective randomized trial. Combined postoperative radiotherapy and weekly cisplatin infusion for locally advanced squamous cell carcinoma of the head and neck: preliminary report of a randomized trial. Combined chemotherapy and radiation therapy in advanced inoperable squamous cell carcinoma of the head and neck: the final report of a randomized trial. Placebo-controlled randomized trial of infusional fluorouracil during standard radiotherapy in locally advanced head and neck cancer. Chemotherapy added to locoregional treatment for head and neck squamous cell carcinoma: three meta analyses of updated individual data. The local-regionally advanced nasopharyngeal carcinoma jigsaw puzzle: where does the chemotherapy piece fit Postoperative radiation therapy for cervical lymph node metastases from an occult squamous cell carcinoma. Th e incidence ofattributes used to define indications forradioth erapy K ey Populationorsubpopulation A ttribute Proportionof Q uality of R eferences N otes ofinterest population inform ation w ith attribute 0 Allregistrycancers M elanom a 0. Since this study will be used in the planning of radiotherapy facilities in Australia, the recommendations of the Australian guidelines have been given precedence over the other guidelines. This includes melanomas of the vagina, anus, oesophagus, nasal cavity and sinuses, oral cavity and other miscellaneous sites. Therefore the decision tree indicates that all mucosal melanomas should be considered for recommendation of radiotherapy, although this is likely to be an over-estimate as an occasional early mucosal melanoma might be considered resectable. Given the rare nature of these lesions, this will not have a significant impact on the estimate of the overall proportion of patients needing radiotherapy. Stage Incidence the Stage data for cutaneous melanoma is reproduced with the permission of the Sydney Melanoma Unit and Professor McCarthy. Therefore there may be a difference in stage distribution between the United States and Australia. This may reflect media campaigns for early detection of melanoma in Australia and a greater awareness of melanoma. To reflect Australian conditions, the Sydney Melanoma Unit data was used as the most relevant source of data. Therefore, it would be reasonable to recommend consideration of radiotherapy for all cases of desmoplastic melanoma. While it is accepted that there will be some patients with poor performance status and/or co-morbidities that exclude them from consideration for adjuvant radiotherapy, there was no available data on performance status correlated with histological type of melanoma. Therefore for the purposes of this decision tree it was assumed that all patients with melanoma with desmoplastic features are considered for radiotherapy. The incidence of desmoplastic melanoma in the South Australian Hospital Registry (5) was 1. Melanoma depth and adjuvant radiotherapy for T4 head and neck melanoma South Australian Hospital Registry data (5) indicate that 90% of melanomas were pT1-3 and 10% were pT4. Therefore, it was considered unnecessary that all pT4 melanomas receive routine radiotherapy. Expert opinion (Dr Hughes, melanoma surgeon, personal communication) suggests that the use of radiotherapy could be reserved for pT4 lesions on the head and neck where there is difficulty in achieving clear deep surgical margins (due to the thin tissue in areas of the head and neck) and the need for conservative surgery to maintain function. Therefore, for the purposes of the decision tree, head and neck melanomas were treated differently from melanomas in sites other than head and neck whereby the pT4 lesions were recommended radiotherapy. Similar data from Australia suggests better local control with adjuvant radiotherapy for node positive melanoma (15) (16) (17). This could be interpreted as consideration of radiotherapy if > 1 node is involved, whereas others (18), M.
Lyme Disease Overdiagnosis: Cause and Ab scess: New Co n ce p t s in Dia gn o sis cholesterol and high blood pressure purchase cheap atorlip-10, Ma n age m e n t cholesterol percentage chart order genuine atorlip-10 online, Cu r cholesterol medication effects purchase atorlip-10 10 mg line. Over 50%of staph in fect ion s occur w ith in 2 w eeks post-sh un t cholesterol vegetable oil order atorlip-10 10mg visa, 70%w ith in 2 m os cholesterol medication for triglycerides purchase atorlip-10 10 mg online. La t e i n f e c t i o n (> 6 m o n t h s a f t e r p r o c e d u r e) Risk: 2 cholesterol jama discount atorlip-10. May also present as shunt malfunction; 29%ofpatients presenting with shunt malfunction had positive cultures. Distal in fect ion of ven triculoperiton eal sh un ts m ay m im ic acute abdom en. Rapid antigen tests used for community acquired meningitis are usually not helpful for the organisms that tend to cause shunt infections. Treatment with antibiotics without shunt removal is therefore recommended only in cases where the patient: is term inally ill, is a poor anesthetic risk, or has slit ventricles that m ight be di cult to catheterize. Re m o v a l o f s h u n t h a r d w a r e In m ost in st an ces, d u r in g t h e in it ial t reat m e n t w it h an t ibiot ics t h e sh u n t is eit h er exte r n al ized. If t h ere is an abd om in al p seu d ocyst, t h e flu id sh ou ld be d rain ed t h rough t h e p erit on eal cat h et er before removing it. Managing vent riculoperit oneal shunt s in pat ient s w it h perit onit is Peritonitis m ay occur as a result of: 16 1. This can be accom plished by reopening the skin in cision used for inserting the peritoneal catheter, and making a second incision over the shunt tub ing, well above this entry point. The cathe ter is grasped at the lower incision and is pulled, extracting both ends (the peritoneal end and the end just cut). Th e se p a r a m e t e r s ca n su gge st t h e d ia gn o sis b u t sh o u ld n ot b e r elie d u p o n exclusively. Th e r e fo r e 44 a single catheter may be employed as long as clinically required. Intraoperative mild hypothermia (as commonly occurs in the operating room) may also increase the risk of wound infection (as demonstrated with colorectal 46 resection). Risk fac tors include: advanced age, obesity, immunosuppression, systemic infection at the time of surgery. In sep t ic cases, variou s m ech an ism s for in fect ion h ave bee n p rop ose d: d irect in ocu lat ion at t h e time of surgery, infection following aseptic necrosis of disc material Pat hogens Se e Ta b le 2 1. Enteric flora in post-op discitis may due to unrecognized breach of the anterior longitudinal ligament with bowel perforation. Fo r cu lt u r e t e ch n iq u e s, se e su r gica l m a n a ge m e n t se ct io n b elow. All p a t ie n t s e ve n t u a lly b e co m e p a in fr e e (o r s ign ifica n t ly im p r o ve). No di erence in outcome was found for the various activity restrictions specified, except for ear lier pain relief w ith first two types listed above. Mo st in fe c tions are due to contiguous spread (usually from an infected air sinus, occasionally from scalp 56 abscess) or to penetrating trauma (including surgery and fetal scalp monitors). Tr e at m e n t u s u a lly in vo lve s s u r gica l d e b r id e m e n t o f in fe ct e d skull, biting o infected bone w ith rongeurs until a norm al snapping sound replaces the m ore m uted sound made by rongeuring infected bone. In the case of an infected craniotomy bone flap, the flap usually must be removed and discarded, and the edges of the skull rongeured back to healthy bone. Bo n e s u s p e ct e d o f in fe ct io n s h o u ld b e s e n t fo r cu lt u r e s. Most treatment failures occurred in patients treated with <4 weeks of antibiotics following surgery. Cr a n io p la s t y m a y b e p e r fo r m e d 6 months post-op if there are no signs of residual infection. Th u s, t h e d iscove r y o f o n e o f t h e se co n d it io n s sh o u ld p r o m p t a se a r ch for t h e o t h e r. Many patients improve with antibiotics alone, but some may deteriorate precipitously Ep id e m io lo g y 59 60 In cid e n ce: 0. Th o r a cic le ve l is t h e m o st co m m o n s it e ( 50%), followed by lumbar (35%) then cervical (15%). Clin ic a l fe a t u r e s Usually presents w ith excruciatin g pain localized over spin e w ith ten dern ess to percussion. Radicu lar sym ptom s follow w ith subsequent distal cord findings, often beginning w ith bowel/bladder dis turbance, abdominal distension, weakness progressing to para and quadriplegia. A fu r u n cle (s k in b o il) so m e w h e r e o n t h e b o d y m ay b e id e n t ifie d in 1 5 %. Pat hophysiology of spinal cord dysfunction Alt h o u gh s o m e co r d sym p t o m s m ay b e d u e t o m e ch a n ica l co m p r e ssio n (in clu d in g t h a t d u e t o ve r t e 65 bral body collapse), this is not always found. A va s cu la r m e ch a n ism h a s a ls o b e e n p o st u la t e d, a n d 59 various com binations of arterial and venous pathology have been described (one autopsy series showed little arterial compromise, but did show venous compression and thrombosis, thrombophle 66 bitis of epidural veins, and venous infarction and edema of the spinal cord). Occasionally, there may be infection of the spinal cord itself,possibly by extension through the meninges. Blo o d cu lt u r e s: m a y b e h e lp fu l in id e n t ify in g o r g a n is m in s o m e ca s e s. Ra d io g r a p h ic s t u d ie s Plain film s Usually n orm al un less th ere is osteom yelit is of adjacen t ver tebral bodies (m ore com m on in in fec tions anterior to dura). Ty p i c a l f i n d i n g s: T1 W I > hypo or iso-intense epidural mass, vertebral osteomyelitis shows up as reduced signal in bone. Vertebral osteomyeli this shows up as increased signal in bone, associated discitis produces increased signal in disc and loss 77 of intranuclear cleft. In m o s t ca s e s, t r e a t m e n t co n s is t s o f e a r ly s u r g ica l e va cu a t io n co m b in e d w it h a n t ib io t ics as the treatm ent of choice. Th e r e fo r e it h a s b e e n r e co m m e n d e d 80 62 that nonsurgical management be reserved for the following patients (reference modified): 1. Su rg e r y Goals are establish in g d iagn osis an d cau sat ive organ ism, d rain age of p u s an d d ebr id em en t of gran u lation tissue, and bony stabilization if necessary. Post-op drainage is not necessary in cases with only granulation tissue and no pus. For 83 recurrent infections, reoperation and post-op suction-irrigation may be needed. Patients w ith associated osteomyelitis of the vertebral body m ay develop instability after lam inec 84 tomy alone especially if significant bony destruction is present. With purulent osteomyelitis, m etal hardware is not contraindicated (titanium is m ore resistant to harboring bacteria than stainless steel for several reasons, including the fact that tita nium does not permit bacteria to form a glycocalyx on its surface), but bone grafting may run the risk of perpetuating the infection. In this situation, some surgeons use beads of calcium sulfate bone void filler impregnated w ith antibiotic. Lo n ge r t h e r 21 apy may be warranted in complicated infections and for patients who have spinal implants or hard ware. Mortality is usually due to original focus of infection or as a complication of residual paraplegia. Often associated with discitis, which may be grouped together under the term spondylodiscitis. Ve r t e b r a l b o d y c o l l a p s e a n d k y p h o t i c d e fo r m i t y m a y o c c u r w i t h p o s s i b l e r e t r o p u l s i o n o f n e c r o t i c bone and disc fragments, compressing the spinal cord or cauda equina. The lumbar spine is the most common site, followed by thora 88 cic, cervical and sacrum. Se n sor y involvem ent is less com m on than m otor and long-tract signs because compression is prim arily anterior. Pot ent ial rout es of spread Th r e e m a in r o u t e s: a r t e r ia l, ve n o u s, a n d d ir e ct e x t e n sio n: 1. Psoas abscess is common (the psoas major muscle attaches to the bodies and intervertebral discs from T12-L5). Definitive diagnosis requires the identification of acid fast bacilli on culture or Gram stain of biopsy material (may be done percutaneously). The infection itself rarely extends into the spinal canal, how ever, epidural granulation tissue or fibrosis or a kyphotic bony deformity may cause cord 97 compression. Surgery may be more appropriate when definite 99 cord compression is docum ented or for complications such as abscess or sinus form ation or spinal instability. Cu lt u r e s / b io p s y Cu lt u r e: b lo o d (p o s it ive in 50%), urine and any focal suppurative process. May be helpful even ifblood cultures are positive (di erent organ 101 ism s retrieved in 15%) an attempt at direct culture from the involved site should be made. Im a g in g A co m p a r iso n o f se n s it ivit ie s a n d sp e cificit ie s o f va r io u s im a gin g m o d a lit ie s is sh ow n in Ta b le 2 1. Earliest changes are loss of cortical endplate margins and loss of disc space height. Bone scan may occasionally be helpful if the diagnosis is still uncer tain when suspicion is high c) percutaneous needle biopsy w ith cultures: usually by radiologist. Characteristics of potential candidates for non-surgical treatm ent are listed in Ta b le 2 1. In d icat ion s for n e u rosu rgical in t er ven t ion (n ote: in t e r ven t io n by a gen e ral su rge on m ay b e in d i cated for empyem a, psoas abscess): 1. Discu ssed b e low Post-op discitis: Can occur follow ing a num ber of procedures; see Postoperative discitis (p. Th is is cove r e d u n d e r p o s t o p in fe ct io n s Many radiographic features of spondylodiscitis and tumor (metastatic and primary) are similar, but tumors rarely involve the disc space, whereas most infections begin in, or before too long, involve the disc space; for more details, see Di erentiating factors (p. Co m m o n p r e s e n t a t io n in y o u n g ch ild r e n: r e fu s a l t o w a lk o r s t a n d p r o g r e ss in g t o r e fu s a l t o s it. Su rger y is reser ved for t h e rare case t h at p rogresses in sp it e of an t ibiot ics, for sp in al in st ab ilit y, or for r e cu rr e n t cases. Uses either technetium-99 (abnormal as early as 7 days following onset of clinical symptoms) or gallium-67 (abnormal within 14 days). A positive scan shows focal increased uptake in adjacent endplates, and m ay be di erentiated from osteomyelitis which will involve only one endplate. A positive scan is not specific for infection, and m ay also occur w ith neo plasms, fractures, and degenerative changes. Cu lt u r e s: An a t t e m p t sh o u ld b e m a d e t o o b t a in d ir e ct cu lt u r e s fr o m t h e in volve d d isc s p a ce. Blo o d cu lt u r e s m a y b e p o s it ive in 50%of cases, and can be helpful in guiding choice of antimi crobial agent when positive. Pat hogens St a p h ylo co ccu s a u r e u s is t h e m o st co m m o n o r ga n ism w h e n d ir e ct cu lt u r e s a r e o b t a in e d, fo llow e d by S. Most patients are started on strict bed rest, and are then mobilized with or without a brace as tolerated Sp in a l b ra cin g Probably does not a ect final outcome. A ords earlier pain relief for some, and may allow return to activity at an earlier time.
The evidence investigating a possible association between calcium intake and cardiovascular outcomes has conflicting findings cholesterol levels chart south africa generic atorlip-10 10mg fast delivery, although cholesterol levels shrimp cheap atorlip-10 10mg on-line, if dietary calcium intakes are adequate xanthoma cholesterol spots safe 10mg atorlip-10, many clinicians prefer to supplement with vitamin D only because of patient concerns and other minor side effects attributable to calcium supplementation (such as constipation and renal calculi) as these may influence adherence cholesterol values normal best 10 mg atorlip-10. There is some heterogeneity in studies between type of vitamin D cholesterol alcohol cheap atorlip-10 10mg amex, route of administration and the dose cholesterol food indian buy discount atorlip-10 10mg on-line, whether daily or as a bolus, and the population (free living or institutionalised) and there have been different conclusions according to the fracture site. The higher-quality trials conclude that calcium is required in addition to vitamin D for antifracture efficacy. However, it is impossible to separate whether it is calcium or high-dose vitamin D that is important, as the trials in the meta-analyses which gave the higher doses of vitamin D also included calcium. R Calcium and vitamin D supplements may be considered to reduce the risk of non-vertebral fractures in patients who are at risk of deficiency due to insufficient dietary intake or limited sunlight exposure. People who have low or no exposure to the sun, for example those who cover their skin for cultural reasons, who are housebound or confined indoors for long periods should be considered at risk of vitamin D deficiency. If dietary calcium intake is adequate (700 mg/day) vitamin D only may be preferred as the osteoporosis treatment adjunct. A small number of studies have provided head-to-head comparisons between different drugs in an attempt to estimate the magnitude of benefit attributable to each medication. In addition, several meta-analyses using indirect comparison methods have been published, which attempt to provide a hierarchy of likelihood of effect across multiple drugs or doses. Such indirect comparisons are subject to greater bias (especially selection bias) than head-to-head randomised comparisons, as the benefit of randomisation does not hold across trials. Direct and indirect comparisons between different drugs used for the treatment of osteoporosis or prevention of fractures are discussed in this section. There was some potential for bias in both studies because of large differences between groups in missing data, which may have confounded the results, and because of the lack of blinding. A meta-analysis compared the clinical effectiveness and safety of subcutaneous denosumab at 60 mg every six months to alendronic acid at 70 mg once weekly. Four suitable studies with vertebral fracture outcomes of at least one year duration were included. Two of these compared denosumab directly with alendronic acid while the other two also included a placebo group. The teriparatide group had significantly fewer new vertebral fractures over an 18 month treatment period (9. Indirect comparisons Indirect comparison has been carried out in an attempt to rank drugs by their effectiveness in preventing vertebral, non-vertebral and hip fractures. Studies have tended to combine effect size with the degree of standard error using pooled data for individual drugs in comparison with placebo for prevention of fractures. These studies are weakened by not taking into account factors which are important in routine clinical decision making, such as risk of harms, ability to tolerate the drug and cost. Because the bone remodelling process is important in maintaining a healthy skeleton by repairing microdamage, there is a theoretical concern that prolonged treatment could in some circumstances, have a detrimental effect on the skeleton. This is especially relevant for bisphosphonates which are the most widely used treatments for osteoporosis. Due to their chemical structure, bisphosphonates bind to bone mineral and exert inhibitory effects on osteoclastic bone resorption which can extend for months or years after treatment has been stopped. Defining the optimal duration of bisphosphonate treatment is therefore relevant to weigh up the risks and benefits of treatment. The same comments apply to other antiosteoporosis medications, although the effects of these wear off much more quickly when treatment is stopped. Eligible patients were required to have been on treatment for at least three years, but those with a femoral neck T-score of less than -3. At baseline around 30% of patients had prevalent vertebral fractures; 30% had femoral neck T-scores below -2. Of the 1,099 included participants, 437 were randomised to placebo, 329 to alendronic acid at 5 mg and 333 to alendronic acid at 10 mg. Treatment was continued for five years, at which point 553 (84%) patients in the alendronic acid groups were analysed compared with 361 (82%) in the placebo group. There was no significant difference between the groups in non-vertebral fractures or morphometric vertebral fractures but clinical vertebral fractures were fewer in the groups who had been randomised to alendronic acid. There was no significant difference in adverse effects between the placebo and alendronic acid treatment groups. R Alendronic acid may be continued for up to 10 years in postmenopausal women with osteoporosis, especially those that are at high risk of vertebral fracture. A further open-label extension of this study analysed fractures in patients in the risedronate group who continued treatment for a further two years, while those in the placebo group were switched onto risedronate. The incidence of new morphometric vertebral fractures during years six to seven in the risedronate group 2+ was 3. The rate of new morphometric fractures in the patients that were formerly on placebo fell from 7. During the fourth year, vertebral fractures occurred in 42/361 of patients in the former placebo group (11. Non-vertebral fractures were similar in the former placebo group (18/361, 5%) and the former risedronate group (19/398, 4. R Risedronate may be continued for up to seven years in postmenopausal women with osteoporosis. Of 2,629 potentially eligible patients 1,223 (46%) were enrolled into the extension. They were randomised to receive three further infusions of zoledronic acid or placebo over three years. There was no significant 1++ difference between the treatment groups in non-vertebral fractures (8. Morphometric vertebral fractures were less common in the zoledronic acid group (3% v 6. Adverse effects that were more common in the zoledronic acid group included a rise in serum creatinine (2. Myocardial infarction and stroke when combined were also more common in the zoledronic acid group (p=0. Hypertension (reported as an adverse event) was more common in the placebo group (15. In the absence of studies investigating further therapy for patients after a three year period without treatment, a review of fracture risk should be carried out to determine whether zoledronic acid should be restarted. R Zoledronic acid may be continued for three years in postmenopausal women with osteoporosis. After an interval of at least three years without treatment, fracture risk may be reassessed to determine the need for further therapy. The authors conclude that four years of strontium therapy is effective in reducing vertebral fracture risk and that protection continues for one year after stopping therapy. R Strontium ranelate may be continued for up to 10 years in postmenopausal women with severe osteoporosis when other treatments are unsuitable. Those who received placebo during years one to three were changed to denosumab during years four and five. The type and numbers of adverse events in the extension study were similar to those in the original study. The authors concluded that denosumab is safe and effective for up to five years for the treatment of postmenopausal women with osteoporosis. There are methodological concerns with this study due to differences between the baseline characteristics in the crossover group and the long-term denosumab group. The evidence in this section is from studies in which various monitoring procedures have been evaluated with regard to their ability to predict the risk of fractures. The results must be interpreted | 71 Management of osteoporosis and the prevention of fragility fractures with caution, however, due to a high risk of bias owing to the retrospective study design and the fact that + 2 studies with different ibandronic acid doses and modes of administration were combined. This study only included the women treated with strontium ranelate and had no comparator group. A linear relationship was demonstrated whereby greater reductions in osteocalcin correlated with greater reductions in vertebral fracture risk. The treatments that are used for osteoporosis do not typically result in a symptomatic improvement and patients seldom gain a tangible benefit from taking the medication. On the contrary, many treatments have complicated instructions for dosing to ensure adequate absorption and some can be associated with adverse effects. Accordingly ensuring that the patient adheres to medication represents a significant hurdle in the effective management of patients with osteoporosis. A significant relationship was evident between the type of message and persistence. One trial randomised 240 women (T-score -2) into four groups to study the association between providing education and feedback about bone marker measurements and persistence with alendronic acid. Overall persistence was 54% at 12 months and there was no significant difference in the four groups. Fifty one per cent of the education group stated that this education affected their decision to remain on treatment. This Asian population from five countries had a high adherence rate which may not be generalisable to other countries. This study was very small (75 patients divided into three groups) and was underpowered for persistence but there was a trend towards better persistence in the monitored group (25% longer). In general, the studies on compliance showed a benefit and those on persistence did not. The method and techniques used to assess compliance and persistence to medication, as well as the type of intervention provided have the potential to affect the results obtained. R Interventions by healthcare professionals, with or without feedback of biomarker results, aimed at improving adherence are recommended in patients who are being given drug treatment for osteoporosis. The g statistic for each group from each study was calculated as the change score difference (absolute or relative) in the exercise group minus the change score difference in the control group, divided by the pooled standard deviation of 1+ the exercise and control groups. Men should aim to consume a healthy balanced diet which contains adequate intake of dietary calcium and vitamin D (see section 6. Many of the treatments that have been used in postmenopausal osteoporosis have also been investigated in men with osteoporosis. Few studies have been designed to investigate the effects of osteoporosis medications on fracture incidence in men. The Scottish Medicines Consortium has not assessed the cost effectiveness of bisphosphonates in men as the manufacturers of branded products declined to make a submission. However, non-proprietary preparations have subsequently become available at lower cost. For the purposes of this guideline, osteoporosis in men is defined by a T-score of -2. Quantitative morphometric analysis indicated significantly fewer vertebral fractures in the alendronic acid group than the placebo group (0. There was no significant difference between the numbers of non vertebral fractures observed in the alendronic acid and placebo groups (5. Morphometric vertebral fractures occurred in 2/191 of the risedronate group and 0/93 of the placebo group. One study investigated the effects of zoledronic acid or placebo in 2,127 men and women who had suffered a hip fracture (see section 6. There was no significant difference in the occurrence of non-vertebral fractures which occurred in 5/588 (0. Furthermore, angina or coronary artery disease was reported more in patients taking strontium ranelate (8. In this study among men there seems to be a benefit in reducing pain interfering with sleep but this must be balanced against a higher rate of adverse events. The intervention and placebo groups both received calcium and vitamin D supplements. Bone mineral density at the spine, ++ 1 hip and wrist increased in the denosumab group as compared with placebo. Treatment allocations were placebo (n=147), 20 micrograms of teriparatide daily (n=151) or 40 micrograms of teriparatide daily (n=139). The trial was terminated prematurely because of preclinical studies which showed that lifelong teriparatide increased the risk of osteosarcoma in rats. However, subsequent clinical studies and preclinical primate studies have shown no evidence to suggest that this risk is observed in humans treated with teriparatide. Because the study was terminated prematurely 1+ the duration of treatment was highly variable ranging from two to 15 months with median treatment duration of 11 months. Bone mineral density increased to a significantly greater extent at the spine (mean 5. Non-vertebral fractures occurred in 3/147 of the placebo group, 2/151 of the 20 micrograms group and 0/139 of the 40 micrograms group, differences that were not significant. There is insufficient evidence to recommend the use of teriparatide for the prevention of fragility fractures in men with osteoporosis. Two systematic reviews have provided evidence on the effects of exercise on bone density. The lack of head-to-head comparisons of interventions makes the choice between interventions difficult for clinicians and patients. Exercise is assumed to be a safe intervention, but consideration must be given to the perceived risks or concerns such as fracture or other injury that some individuals may have when starting or resuming exercise.
If lesion is suspected in the intervertebral foramen it may be nec essary to carry the removal of bone well out to the side cholesterol medication buy generic atorlip-10 10mg online, even taking in part of the pedicle cholesterol levels vary day to day atorlip-10 10mg with visa. It frequently comes away without any dissection and if not no cholesterol in eggs order atorlip-10 in india, section across its base or removal with curette is bloodless cholesterol ratio us buy generic atorlip-10 on-line. Though we have done it in only two cases cholesterol levels in food chart trusted atorlip-10 10mg, we believe that it may be advisable to slip bone chips in between the stumps of the laminae before closing the wound cholesterol lowering vegetarian diet cheap atorlip-10 10mg fast delivery, in order to facilitate fusion. After removal of the tor piece of the disc one frequently finds an opening through which a probe may be passed into the nucleus pulposus. We conclude from this study: a that herniation of the nucleus pulposus into the spinal canal, or as we prefer to call it, rupture of the interver tebral disc, is a not uncommon cause of symptoms. That the lesion frequently has been mistaken for cartilaginous neo plasm arising from the intervertebral disc. That the treatment of this disease is surgical and that the results obtained are very satisfactory if compression has not been too prolonged. The disc was thereaf termaderesponsibleforallkindsofbackandlegpainandmanytreatmentfail ures were the consequence. Therefore, his ap proach served also as a precursor to the microscopically assisted approach [73]. Lyman Smith introduced the American physician Lyman Smith developed a less invasive method for chemonucleolysis disc protrusions and reported his results in 1964 [109]. He injected chymopapain for disc prolapses into the disc to shrink the disc protrusion. Although chemonucleolysis was effec tive, this method went out of fashion because of some cases of anaphylactic reac tion and transverse myelitis. Caspar and Williams In 1975, Hijkata of Japan first reported on a percutaneous lumbar nucleotomy introducedmicrodiscectomy technique by a posterolateral approach [35]. In the late 1970s, the German neuro surgeon Caspar and the American neurosurgeon Williams introduced the use of the microscope for minimally invasive discectomy, which today has become the standard technique in many centers [17, 123]. Ascher performed the first percutaneous laser decompression of intervertebral discs [14], but this technique never demonstrated clinical efficacy. History of Spinal Disorders Chapter 1 21 A further milestone in the treatment of degenerative disc disease was the devel U. Fernstrom implanted opment of an artificial disc, which allowed lumbar motion to be preserved. Spinal Stenosis the first evidence of spinal stenosis can be found in Egyptian mummies. He observed at autopsy three specimens with narrowing of stenosis in 1803 the spinal canal [93]. He was also able to relate the pathological findings to the typical clinical symptoms of spinal stenosis. In his article, published in the Lan cet in 1927, Putti gained international attention and it was a further step in the understanding of the pathomechanism of sciatica in cases which are not caused by a slipped disc [95]. He introduced the concept of developmental stenosis, which is caused by an abnormally short midsagittal diameter of the spinal canal [114, 115]. Spinal Infections Despite the advent of chemotherapy and improved surgical techniques, spinal infections are still a potentially life threatening disease even in the industrialized world. Egyptian Mummies and Sir Percival Pott Spinal tuberculosis is older Spinal tuberculosis is older than written history, because the first evidence of spi than written history nal tuberculosis was found in a skeleton from about 5000 B. Further evi dence of spinal infection most likely caused by tuberculosis was found in Egyp tian mummies dating from the Predynastic time, 3000 B. A very good example of spinal tuberculosis was found in Neshparenhan, from the cache of 44 priests of Amun (21st Dynasty, 1100 B. But after some brief enthusiasm, this treatment was abandoned because of various severe complications. He published his account of tuberculous para plegia entitled Remarksonthatkindinpalsyofthelowerlimbs,whichisfre quently found to accompany a curvature of the spine, and is supposed to be caused by it (Fig. Spinal infection a the Old Egyptian mummy Neshparenhan, a priest of Amun (circa 1100 B. He showed that there was not a luxation of vertebrae but an inflammatory abscess that compromises the spinal cord. Treatment Before the 19th century, treatment was just based on bed rest and/or cruel trac tion. Spinalframesand,later,plasterbeds, plaster jackets and back supports came into almost universal use but without any proven benefit. Despite the first experience of abscess drainage reported by Pott, this proce dure seemed to be very dangerous because of the high death rate leading to con troversies. With the advent of new surgical and supporting techniques in the late 19th century, more and more surgical approaches to the treatment of tuberculo Lange was a pioneer sis were developed. Albee tried to stabilize the spine of a patient suffering from spinal tuberculosis. He first sagittally split the spinous processes, and then he laid a strip of autologous tibia between the two halves of them [1]. During this time, Albee was very interested in bone graft techniques and he therefore performed many bone graft experiments on dogs. Hodgson and his coworkers suggested a new surgi cal technique which consisted of: radical surgical debridement anterior spinal fusion with autologous bone-graft (rib, ilium) [58] chemotherapy In the 1950s, although the first effective chemotherapies with streptomycin, iso niazid and paraamino-salicyclic acid were successful in the treatment of pulmo narytuberculosis,orthopedicsurgeonsweresuspiciousoftheeffectivenessfor spinal tuberculosis [65, 88]. Based on the experience of the Hong Kong school, radical debridement, fusion and chemotherapy became the gold standard for cases with deformity and neurologic compromise [82]. Ankylosing Spondylitis Ankylosing spondylitis is a highly heritable, common rheumatic condition, primar ily affecting the axial skeleton. There is still no causative cure and for patients it remains a very disabling disease (Fig. The first evidence of ankylosing spondy litis was found in many Egyptian mummies ranging from 3000 B. Ankylosing spondylitis a Typical features of ankylosing spondylitis in the skeletal remains of a Late Medieval/Early Modern Times male 50 years of age from La Neuveville, Switzerland. He was one of the most powerful Egyptian kings ever and is remem bered for his countless monuments, for example the temple in Abu Simbel [81]. In 1693, he described an unusual skeleton consisting of a unified spine that was found in a local cemetery (Fig. He suggested that the deformity originated in utero as a consequence of pressure from abscess tumor in the womb or elsewhere. First clinical reports of two putative cases of ankylosing spondylitis were both published in early issues of the Lancet. For the first time, the whole complex of ankylosing spondylitis was described fully and at length in 26 Section History of Spinal Disorders d Figure 9. Petersburg, was interested in ankylos ankylosing spondylitis ing spondylitis (Fig. With his report on ankylosing spondylitis in 1893, he in Continental Europe made it very popular in Europe [117]. But he misconceived the etiology of ankylosing spondylitis, because he believed that the spinal stiffness was caused by a neurological disorder. He also postulated that the etiol ogyofankylosingspondylitisisanosteopathycausedbyinfectionortoxin, which finally leads to a hyperostotic process of the facet joints. Spinal Injuries Spinal injuries have been diagnosed and treated since antiquity and are still one Spinal injuries have been of the most severe injuries which lead to handicap and disability. In the past, diagnosed and treated most of the patients with spinal cord injuries died after a short time because of a since antiquity combination of pressure sores and urinary tract infection. A first description of spinal cord injuries is found in the Edwin Smith Surgical the Edwin Smith Papyrus Papyrus [10]. The manuscript, written on papyrus, is dated to the 16th cen gives the first description tury B. Butitiswidelybelievedthatitisacopyof of spinal injuries a much earlier work possibly 1000 years older. In this text, collections of different instructions are found concerning for example a crushed cervical vertebra or cer vical displacement of a vertebra. Hippocrates provided According to the Hippocratic orthopedic textbook On Articulations, spinal inju the first classification ries are classified into three different types [57] based on the direction of verte of spinal injuries brae displacement and the spine deformity: anterior displacement posterior displacement injuries with no visible deformity Each of these types is described with their prognosis. Additionally, Galen performed different experiments on spinal knowledge of neurological cord and spinal cord lesion in primates as outlined above, and he also made topography observations on patients with spinal injuries notably gladiators falling from chariots, perhaps the earliest recorded spinal injuries from road accidents. On this basis, Galen was able to diagnose the level of the injury by observing the par alyzed muscles and the area of sensational loss. Littre, who published the whole work of Hippo cratesofCosinthefirsthalfofthe19thcen b tury. The medi problems related to the spine cal textbook On Railway and Other Injuries of the Nervous System published by John Erichsen in 1866 was fully devoted to this subject [32]. There was great public and medical debate on railway spine and its enormous amount of compensation. This culminated for example in the medical advice of the Lancet Commission on the railway spine in 1862 [66].
Purchase generic atorlip-10 canada. Tips to Understand a Cholesterol Diet Plan.
References
- Melick WF, Naryka JJ, Schmidt JH: Experimental studies of ureteral peristaltic patterns in the pig. II. Myogenic activity of the pig ureter, J Urol 86:46, 1961.
- Donohue RE, Fauver HE: Unilateral absence of the vas deferens. A useful clinical sign, JAMA 261(8):1180n1182, 1989.
- Griesdale DE: Etomidate for intubation of patients who have sepsis or septic shock-where do we go from here? Crit Care 16(6):189, 2012.
- Schier, F. Laparoscopic surgery of inguinal hernias in children: initial experience. J Pediatr Surg. 2000; 35(9):1331-1335.
- Bellmunt J, Guillem V, Paz-Ares L, et al: Phase I-II study of paclitaxel, cisplatin, and gemcitabine in advanced transitional-cell carcinoma of the urothelium. Spanish Oncology Genitourinary Group, J Clin Oncol 18(18):3247n3255, 2000.
- Fathi M, Lundberg IE, Tornling G. Pulmonary complications of polymyositis and dermatomyositis. Semin Respir Crit Care Med 2007;28(4):451-8.