Charles H. Cook, M.D.
- Assistant Professor of Surgery and Critical Care
- The Ohio State University Hospitals
- Columbus, OH
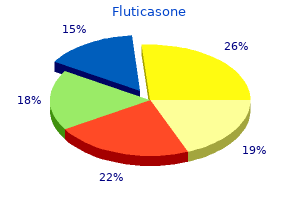
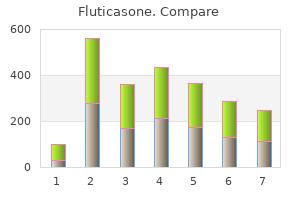
Recommendations for clinical monitoring are summa rized below (Table 2): Table 2: Clinical Monitoring of Bone Marrow Failure Normal/mild marrow failure Blood counts stablefi Marrow: Marrow: every 16 months every year *Persistent drop or rise in blood counts without apparent cause warrants bone marrow evaluation asthma inhalers cheap fluticasone 500 mcg visa. A similar monitor ing regimen is recommended for patients with mildly abnormal asthma treatment with reflexology buy fluticasone from india, but stable asthma symptoms in 7 month old discount fluticasone 500mcg otc, blood counts without any associ ated clonal marrow abnormalities asthma definition cdc buy 250 mcg fluticasone fast delivery. It would be reasonable to examine the blood counts every 12 months and the bone marrow every 16 months initially to determine if the blood counts are stable or progressively changing asthma x ray discount fluticasone online american express. If the blood counts are stable asthma symptoms pregnancy generic 500 mcg fluticasone otc, then the frequency of bone marrow exams may be decreased. Appropriate plans for stem cell transplantation should be in place, as adverse changes may evolve rapidly. Blood counts falling or rising Patients with progressively changing blood counts without a clinically apparent underlying cause. Such patients warrant continued close monitoring with complete blood counts every 12 months and a marrow exam with cytogenetics every 16 months. Appropriate plans for intervention should be in place, as adverse changes may evolve rapidly. Excellent results have been achieved using modifed transplant regimens for matched sibling donor transplants. Currently available alternate donor regimens appear to have markedly improved results so far compared to past regimens, representing a new opportunity for patients. Since it is currently not possible to predict which patients will progress to severe marrow failure, transplantation prior to the development of signifcant marrow failure may unnec essarily subject a subset of patients to both early and late transplantrelated morbidity and mortality. Potential longterm transplantrelated risks such as increased risk of solid tumor development remain to be ascertained. The effects of androgens are most pronounced in the red cells and platelets, but neutrophil counts may also improve. The advantages of androgens include the low risk of therapyrelated mortality and the long history of expe rience with their use; their side effects have been well documented. The major potential side effects associated with androgen therapy are listed in Table 3. About half of all patients treated will respond to androgen therapy, and a subset of those who initially respond may become refractory over time. For patients for whom hematopoietic stem cell transplant is indicated, delay in going to transplant may increase transplantassociated risks. Since there is no evi dence that androgens can forestall bone marrow failure, treatment is initiated when cytopenias drop to clinically signifcant levels but before the marrow becomes com pletely devoid of hematopoietic stem cells for andro gens to stimulate. The standard recommended androgen is oxymetho lone, with a starting dose of 25 mg/kg/day rounded to the nearest 1/4 tablet (50 mg tablets are available in the United States, while 10 mg tablets are available in many countries in Europe). If the patient responds to the initial dose with a stabilization of or increase in the hemoglobin level, the daily dose may be tapered in 1/2 tablet decrements after 3 months. Thereafter, a reasonable taper schedule might involve gradually decreasing the androgen dose at 24 month intervals. The family should be counseled about the possible side effects of androgen therapy and the child, especially teenagers, should be forewarned about them. Every effort should be made to minimize the side effects by tapering the dose whenever possible. Aggres sive acne treatment with topical benzoyl peroxide and topical antibiotics (clindamycin or erythromycin) may make the treatment more tolerable. Since the masculinizing side effects of oxymetholone are particularly troublesome in girls and women, some female patients have been treated with a different androgen, danazol, which is hypothesized to produce fewer of these side effects. It has not been established whether, dose for dose, danazol is as effective and, at the same time, less masculinizing than oxymetholone. Clinical trials comparing effcacy and side effects of different androgens are cur rently being developed. The use of low dose (510 mg every other day) predni sone in an attempt to attenuate the premature epiphy seal closure by androgens has been advocated by some physicians. There are no data to support any sparing of androgen toxicity with the use of low dose predni sone. Furthermore, prednisone therapy carries a risk of 60 Fanconi Anemia: Guidelines for Diagnosis and Management additional bone toxicities, such as avascular necrosis or osteoporosis. Unfor tunately, transaminases do not always correlate with the degree of liver infammation on liver biopsy. If liver transaminases increase to 35 times above nor mal, the androgen dose can be tapered until the blood tests improve. Androgenassociated liver adenomas can resolve after androgens are discontinued, but some may persist even years after androgens are stopped. If screening tests raise a concern for adenocarcinoma, a liver biopsy (generally performed as an open procedure to minimize bleeding risk) should be considered. These formulations offer the advantage of decreased injection frequency (a particu larly appealing prospect for thrombocytopenic patients). A bone marrow aspirate/biopsy with cytogenetics is recommended prior to the initiation of cytokine treat ment, given the theoretical risk of stimulating growth of a leukemic clone. It is reasonable to monitor the bone marrow morphology and cytogenetics every six months while patients are treated with cytokines. There are currently no studies demonstrating a causal relationship between cytokine therapy and leukemogenesis. In the setting of a compelling clinical indication for cytokine therapy, there is no literature to mandate withholding cytokines from patients with clonal abnormalities. Investigational protocols For those patients who fail to respond to androgens or cytokines and have no acceptable transplant donor or pose an unacceptably high transplant risk, investiga tional protocols for new therapies may be considered (see Chapter 12). Early discussion with a transplant expert is recommended to allow families the option of initiating the pro cedure at an optimal time for the patient. If the patient has no hematologic abnormalities at the time of diagnosis, it is reasonable to defer refer ral to a transplant center. A careful discussion with a hematologist and transplant physician is warranted for families interested in this investigational approach. Selection of a donor requires additional confrmatory testing as well as determination of donor availability. This stage accrues a substantial charge and is not undertaken until active plans for transplant are underway. Information regarding the number of potential donors available is helpful in estimat ing the time likely required to complete a full donor search if the marrow failure progresses. Severe marrow failure: Consider unrelated donor hematopoietic stem cell transplant for eligible candidates. Severe marrow failure unresponsive to androgens/ cytokines and high transplant risks: Consider investigational protocols. It remains unclear whether pretransplant chemotherapy improves or worsens out comes. Close monitoring of the hemoglobin is necessary, as outlined above, so that treatment may be instituted before transfusion with packed red blood cells is required. The hemoglobin level at which treatment is started should be modifed upward for patients who live at high altitude, where the normal range for hemoglobin levels is higher. When treatment is anticipated, it should be initiated under the care of a hematologist. As dis cussed above, treatment options for anemia consist of bone marrow transplant or androgens. High transfu sion burden may adversely affect transplant outcomes, so timely consideration of transplant is recommended. Some physicians advocate a more aggressive and regu larly scheduled transfusion program to maintain as nor mal a quality of life as possible for patients with bone marrow failure. These physicians reason that the patient should maximize the beneft of transfusion therapy. Using the latter approach, a patient would be transfused to maintain a minimal trough hemoglobin of 78 g/dl. A posttransfusion hemoglobin level of 1012 g/dl is generally suffcient to allow for normal activity, growth, and development in children. Irradiated blood products should be used to avoid transfusion associated graftversushost disease. Extended antigen matching may be impor tant for patients in certain racial groups, where minor antigen mismatch is more commonly encountered. The use of family members as directed donors may cause alloimmunization to an antigen that would increase the risk of graft rejection after sibling donor hematopoietic stem cell transplant. Secondary iron overload Each mL of transfused packed red cells contains approximately 0. Since the human body lacks mechanisms to actively eliminate excess iron, patients who receive multiple red blood cell transfu sions are at risk for accumulating toxic levels of iron overload. The liver is a primary site of iron accumula tion, and hepatic fbrosis and cirrhosis may result. Cardiac decompensation may be sudden and acute despite regular monitoring with electrocardiograms and measurements of cardiac func tion. Iron also targets endocrine organs such as the pituitary, pancreas, thyroid, and para thyroid (Table 5). Table 5: Clinical Complications of Iron Overload Liver disease with fibrosis and cirrhosis Cardiac failure, arrhythmias Hypopituitarism: central hypogonadism growth hormone deficiency central hypothyroidism Poor growth Diabetes mellitus Primary hypothyroidism Primary hypogonadism Hypoparathyroidism While ferritin levels are often followed as a convenient marker for total body iron load, their interpretation is complicated by additional factors such as acute or chronic infammation and infection or hepatitis. The gold stan dard for the measurement of total body iron has been a liver biopsy; however, hepatic iron distribution may be uneven, particularly with cirrhosis and, thus, liver biop sies may be limited by sampling error. Elevated liver iron >15mg/g dry weight is associated with a high risk of cardiac toxicity. Bleeding or infection as possible complications of the surgical biopsy procedure are of heightened concern in patients who are thrombocyto penic or neutropenic. Guidelines for the institution of iron chelation therapy in bone marrow failure patients are based on those established for thalassemia patients, with the caveat that thalassemia patients who undergo accelerated, albeit ineffective, erythropoiesis, often have concomitant increases in iron absorption and are transfused to the point of suppressing endogenous hematopoiesis. Total red cell volumes transfused, particularly for infants and small children, as well as total body iron status as refected in liver iron, cardiac iron, and ferritin levels must be carefully monitored. As a general guide, chelation is consid ered when the total red cell volume transfused reaches 200mL/kg (roughly corresponds to a total of 1218 red cell transfusions) or the liver iron reaches 7mg/g dry weight. Chronically transfused patients heading to a hematopoietic stem cell transplant may also beneft from total body iron measurements and chelation therapy to reduce iron levels. In situations where liver iron measurements are not clinically available, a serum ferritin persistently greater than 1, 500 without other apparent etiologies has been used as a surrogate, albeit imperfect (see prior discussion), marker. The risk of side effects increases as the dose of chelator exceeds body iron stores. Although generally effective, its use is complicated by the need for parenteral infusion (subcutaneously or intravenously). Furthermore, deferoxamine must be administered over prolonged periods of time since only a small proportion of total body iron is available for chelation at any given moment and the halflife of deferoxamine is short. Subcutaneous infusions pose risks of bleeding or infection in patients with thrombo cytopenia or neutropenia. Side effects of deferoxamine include loss of hearing or vision, particularly when desferoxamine doses are high relative to iron stores. Immediate cessation of deferoxamine and medical evaluation is warranted if such symptoms arise. Defer oxamine therapy is associated with an increased risk of Yersinia enterocolitica infection, and the drug should be stopped for unexplained fevers pending the results of blood cultures and infection workup. Given the disadvantages of a parenterally administered drug, deferasirox offers an attractive alternative for iron chelation. Deferasirox is conveniently administered orally once a day as a slurry on an empty stomach. Clinical experience with deferasirox is limited, but short and longterm side effects reported to date are generally mild. Patients who continue to have unacceptable iron levels on deferasirox despite dose escalation may bene ft from switching back to deferoxamine until goal iron levels have been achieved. Studies suggest that deferiprone may be more effcient than deferoxamine at removing cardiac iron. Its utility is limited by its side effects, which include agranulocytosis, arthritis, and hepatic fbrosis. For patients with severe iron overload or with cardiac functional compromise (arrhythmias or failing left ven tricular function), continuous high dose. Thrombocytopenia Bone marrow transplant should be considered when the platelet counts fall below 50, 000/mm3. If transplant is not pursued, then thrombocytopenia should be treated with androgens as the platelet count declines to 30, 000/mm3.
In ad dition asthma treatment 1960s generic fluticasone 250 mcg without prescription, cultural differences between patients and clinicians or patients and other aspects of the care system may also influence the course and conduct of treatment and require attention asthma 6 step plan fluticasone 500mcg. When a patient with an eating disorder has been sexually abused or has felt helpless in other situations of boundary violations asthma forecast order fluticasone amex, this may stir up needs in the clinician to rescue the patient asthma histology generic fluticasone 250 mcg free shipping, which can occasionally result in a loosening of the therapeutic structure asthma 4 year old boy purchase fluticasone 250 mcg free shipping, the loss of therapeutic boundary keeping asthma definition 18th cheap generic fluticasone uk, and a sexualized countertransference reaction. In some cases, these counter transference responses have led to overt sexual acting out and unethical treatment on the part of the clinician that have not only compromised treatment but also severely harmed the patient (166). The maintenance of clear boundaries is critical in treating all patients with eating disor ders, not only those who have been sexually abused but also those who may have experienced other types of boundary intrusions regarding their bodies, eating behaviors, and other aspects of the self by family members or others. Regular meetings with other team members and/or formal supervision can also help clinicians avoid boundary violations with eating disorder pa tients. However, the license to be informal may create a climate in which a clinician is at a greater risk to violate therapeutic boundaries; such an occurrence must be consistently and carefully prevented. Some clinicians use group psychotherapy as an adjunctive treatment for anorexia nervosa; in such cases, however, caution must be taken that patients do not compete to be the thinnest or sickest patient in the group or become excessively demoralized by observing the ongoing struggles of other patients in the group. For that reason, clinicians sometimes prefer heteroge neous groups that combine patients with bulimia nervosa and those with anorexia nervosa. Some clinicians consider that eating disorders may be usefully treated through addiction models, but no data from short or longterm outcome studies using these methods have been reported. Literature from Anorexics and Bulimics Anonymous and Overeaters Anonymous emphasizes that these programs are not substitutes for professional treatment. These organiza tions specifically recommend that members seek appropriate medical and nutritional guidance. Nevertheless, there are concerns about zealous and narrow application of the 12step philoso phy in addictionoriented programs for eating disorders. Programs that focus exclusively on ab staining from binge eating, purging, restrictive eating, and exercise. Clinicians frequently report encountering patients who, while attempting to resolve anorexia nervosa by means of a 12step program alone, might have been greatly helped by concurrent conventional treatment approaches such as nutritional counseling and rehabilitation, medica tions, and psychodynamic or cognitivebehavioral approaches. By limiting their attempts to re cover to their participation in a 12step program alone, patients not only deprive themselves of the potential benefits of conventional treatments but also may expose themselves to mis information about nutrition and eating disorders offered by wellintended nonprofessionals participating in and sometimes running these groups. Attempts have been made to integrate traditional and 12step approaches into treatment; such approaches can offer a strong sense of community, but the effectiveness and potential adverse effects of these combined interventions have not been systematically studied (167). It is important for programs using a 12step model to be equipped to care for patients with the substantial psychiatric and general medical prob lems often associated with eating disorders. Selective support groups led by professionals and advocacy organizations may be beneficial as adjuncts to other psychosocial treatment modalities. However, clinicians should remain cogni zant of the idiosyncratic recommendations made in some selfhelp groups. Sometimes, participants Treatment of Patients With Eating Disorders 47 Copyright 2010, American Psychiatric Association. Patients and their families are increasingly using online web sites, news groups, and chat rooms as resources. Although substantial amounts of worthwhile information and support are available in this fashion, the lack of professional supervision of these sources may sometimes lead to mis information and unhealthy dynamics among users. Clinicians should ask patients about their use of electronic support and other alternative and complementary approaches and be prepared to openly and sympathetically discuss the information and ideas they and their families have gath ered from these sources. As with any form of intervention, various psychosocial interventions may generate adverse ef fects; however, these have not been systematically studied with regard to treating anorexia nervosa. Some that have been observed by clinicians, patients, and families include 1) fostering negative attitudes in patients and/or families toward health care professionals without adequate discussion and reflection, thereby increasing the risk that patients will drop out of treatment and become less willing to seek or engage in professional treatment; 2) delaying referral to more appropriate inter ventions; and 3) generating burdensome costs without reasonable or expected benefits (13, 168). Most patients are initially resistant to changing their eating behaviors, particularly when it comes to increasing their caloric intake or reducing exer cise. However, the complete lack of acceptance of a psychotherapeutic approach appears to be rare, although this has not been systematically studied. Alternative strategies may be necessary to facilitate the therapeutic process and prevent the abrupt termination of therapy (13). As with all therapeutic interventions, it is essential that the therapist be alert to potential countertransference phenomena toward these often difficultto treat patients. If unresolved, these reactions have a high potential for disrupting or hastening the termination of treatment. The results after 1 year of psycho therapy were modest in all groups, although the psychoanalytic psychotherapy and family ther apy groups fared better than those in the lowcontact, routinecare control group. Nevertheless, many clinicians report seeing patients with chronic anorexia nervosa who, after many years of struggling with their disorder, experience substantial remission; thus clinicians are justified in maintaining and extending some degree of hope to patients and families. For patients whose anorexia nervosa continues to be resistant to treatment despite substan tial trials of nutritional rehabilitation, medications, and hospitalizations, more extensive psy chotherapeutic measures may be undertaken in a further effort to engage and help motivate them or, failing that, as compassionate care. This difficulttotreat subgroup may represent an asyet poorly understood group of patients with malignant, chronic anorexia nervosa. Efforts to understand the unique plight of such patients may sometimes lead to engagement in the therapeutic alliance, thereby allowing the nutritional protocol to be initiated (125, 141, 142, 169, 170). With patients who have difficulty talking about their problems, clinicians have re ported a variety of nonverbal therapeutic methods, such as creative arts and movement therapy programs, to be useful (171), but these methods have not been formally studied. At various stages of recovery, occupational therapy programs may also enhance selfconcept and selfefficacy (172, 173), but again these programs have not been formally studied. The decisions about whether to use psychotropic medications and which medications to choose will be determined by the re maining symptom picture. Many patients with anorexia nervosa are extremely reluctant to take medications and often refuse those that they know to specifically affect weight. These issues must be discussed sympathetically and comprehensively with patients and, for children and adoles cents, with their families. On the basis of several studies, fluoxetine does not appear to confer significant benefits dur ing weight restoration (174, 175), nor did citalopram increase the rate of weight gain in a small study (176). In contrast, in weightrestored patients, fluoxetine in dosages of up to 60 mg/day may decrease relapse episodes and has been associated with better maintenance of weight and fewer symptoms of depression (177). Although higher dosages of fluoxetine have been found to impair appetite and cause weight loss in normalweight and obese patients, this effect has not been reported in anorexia nervosa patients treated with lower dosages. Malnourished patients are also much more prone to the side effects of medications. For ex ample, the use of tricyclic antidepressants may be associated with greater risk of hypotension, in creased cardiac conduction times, and arrhythmia, particularly in purging patients whose hydration may be inadequate and whose cardiac status may be nutritionally compromised. Given Treatment of Patients With Eating Disorders 49 Copyright 2010, American Psychiatric Association. With all antidepressants, strategies to manage side effects include limiting the use of medications to pa tients with persistent depression, anxiety, or obsessivecompulsive symptoms; using low initial doses in underweight patients; and remaining vigilant about early manifestations of side effects. Several other antidepressants have also been associated with significant side effects that are of relevance to the treatment of anorexia nervosa patients. Bupropion has been associated with an increased likelihood of seizures in patients with bulimia nervosa (180, 181); although the reason for this is unknown, it is suspected that patients with anorexia nervosa, bingepurge type, may also be at increased risk for seizures. Thus, this medication is not recommended for patients with anorexia nervosa, particularly those who purge. Mirtazapine, an antidepressant associated with weight gain, has also been associated with neutropenia. In addition, the only pub lished case report of using mirtazapine to treat anorexia nervosa described a patient also taking fluvoxamine who developed the serotonin syndrome (182). Thus, mirtazapine may not be suit able for use in underweight anorexia nervosa patients. Although no controlled studies have been reported in pa tients with anorexia nervosa, controlled trials of olanzapine and risperidone are under way. A small openlabel study of lowdose haloperidol also showed improved insight and weight gain in severely ill patients (198). The quality of the available ev idence on using antipsychotic medications is also limited by the fact that studies rarely include male patients and have included only small numbers of adolescents; in addition, only case re ports are available regarding prepubertal children. If antipsychotic medications are used, the possibility of extrapyramidal symptoms, especially in debilitated patients, should be considered and routinely assessed. None has been shown to have specific value in the treatment of anorexia nervosa symptoms (199). Other medications have been used to address associated features of anorexia nervosa. For example, antianxiety agents have been used selectively before meals to reduce anticipatory anx iety concerning eating (200, 201), and promotility agents, such as metoclopramide, are com monly offered for the bloating and abdominal pains that result from gastroparesis and that contribute to the premature satiety seen in some patients. However, before prescribing meto clopramide, clinicians should consider the fact that extrapyramidal symptoms are more likely to be seen in underweight anorexia nervosa patients. However, no good supporting evidence exists to demonstrate the efficacy of this treatment (202, 203). Only in a subset of verylowweight women (<70% average body weight) did it prevent further bone loss (204). Estrogen can cause the fusion of the epiphyses and should not be administered to girls before their growth is completed (3). This, in turn, may cause the patient to misunderstand that her body is functioning normally and therefore contribute to denial of the need to gain more weight. Clinicians stress that efforts should be made to allow patients to increase their weight and achieve resumption of normal menses before they are offered estrogen (205). There is no indication for the use of biphosphonates such as alendronate in patients with anorexia nervosa. Thus, the recommended treatment for low bone mineral density includes weight gain and calcium with vitamin D supplementation (207). A primary focus for nutritional rehabilitation is to help patients develop a structured meal plan that will allow them to reduce the episodes of dietary restriction and the urge to binge and purge. Because most bulimia nervosa patients who have been studied are of normal weight, nutritional restoration will not be a central focus of treatment. In addition, even if their weight is within statistically normal ranges, many patients with bulimia nervosa weigh less than their appropriate biologically determined set points (or ranges) and may have to gain some weight to achieve physiological and emotional stability. Although many patients with bulimia nervosa report irregular menses, improvement in menstrual function has not been systematically assessed in the available outcome studies. Thus, even among patients of normal weight, nutritional counseling may be a useful adjunct to other treatment modalities in reducing behaviors related to the eating disorder, minimizing food restrictions, increasing the variety of foods eaten, and encouraging healthy but not compul sive exercise patterns (208). Those patients for whom some weight gain is indicated similarly require the establishment of a pattern of regular, nonbinge meals, with attention on increasing their caloric intake and expanding macronutrient selection. Patients with bulimia nervosa who are overweight or obese have not been well studied. Behavioral techniques, such as planned meals and selfmonitoring, may also be helpful for managing initial symptoms and interrupting bingepurge behaviors (213, 214). It should be pointed out that these study results may not be generalizable to typical clinical situations. It is also possible that the narrow inclusion cri teria of some studies limit the generalizability of the study results (216). These approaches address developmental issues; identity formation; body image concerns; self esteem; conflicts surrounding sexuality, anger, or aggression; affect regulation; gender role ex pectations; interpersonal conflicts; family dysfunction; coping styles; and problem solving. Some bulimia nervosa patients, particularly those with concurrent personality pathology or other cooccurring disorders, may require substantially longer treatment. Also unknown is how the length and characteristics of the treatments varied according to other clin ical dimensions of these patients. Exactly what is required over the long run to best help patients resolve lingering preoccupations with body image and the more subtle but impairing psycholog ical dimensions that may be associated with eating disorders requires additional study. These concerns are often approached in practice through a variety of longerterm psychotherapies. Family therapy should be considered whenever possible, especially for adolescents still living with parents or for older patients with ongoing conflicted interactions with parents. Support groups and 12step programs such as Overeaters Anonymous may be helpful as ad juncts to initial treatment of bulimia nervosa and for subsequent relapse prevention but are not recommended as the sole initial treatment approach for bulimia nervosa (168, 223). As noted above, these support organizations emphasize in their literature that their programs are not sub stitutes for professional treatment and specifically recommend that members seek appropriate medical and nutritional guidance. However, clinicians should remain cognizant of the idiosyn cratic recommendations made in some selfhelp groups.
Fluticasone 500mcg on-line. Concordia Visiting Nurses Home-Based Pulmonary Rehab.
Syndromes
- Women have decreased levels of estradiol and other estrogen hormones after menopause.
- EKG (electrocardiogram or heart tracing)
- For hemolytic anemia caused by an overactive immune system, drugs that suppress the immune system may be used.
- Very low blood pressure
- Genetic factors
- Spine surgery, including diskectomy, foraminotomy, laminectomy, and spinal fusion
- Endoscopy to remove the battery if it has been swallowed and is still in the esophagus or stomach
References
- Hemann MT, Bric A, Teruya-Feldstein J, et al. Evasion of the p53 tumour surveillance network by tumour-derived MYC mutants. Nature 2005;436(7052):807-811.
- Nakano S, Ikata T, Kinoshita I, Kanematsu J, Yasuoka S. Characteristics of the protease activity in synovial fluid from patients with rheumatoid arthritis and osteoarthritis. Clin Exp Rheumatol 1999; 17:161-70.
- Shaver PJ, Carrig TF, Baker WP. Postpartum coronary artery dissection. Br Heart J. 1978;40:83-86.
- Beltrami AP, Urbanek K, Kajstura J, et al. Evidence that human cardiac myocytes divide after myocardial infarction. N Engl J Med 2001;344:1750-1757.
- Behcet H. Uber rezidivierende, aphtose, durch ein Virus verusachte Geschwure am Mund, am Auge und an den Genitalien. Dermatologische Wochenschr 1937;105:1152-7.
- Khaw AL, Barrett-Connor E. Dietary potassium and strokeassociated mortality: A 12-year prospective study. N Engl J Med 1987;316:235.
- Ammash N, Warnes CA: Cerebrovascular events in adult patients with cyanotic congenital heart disease, J Am Coll Cardiol 28:768-772, 1996.