Ramon L. Ruiz, DMD, MD
- Medical Director, Pediatric Craniomaxillofacial Surgery
- Vice Chair, Department of Children? Surgery
- The Arnold Palmer Hospital for Children
- Associate Professor of Surgery,
- University of Central Florida College of Medicine
- Orlando, Florida
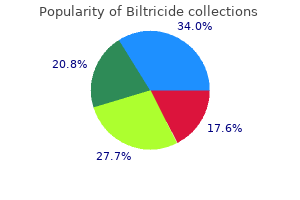
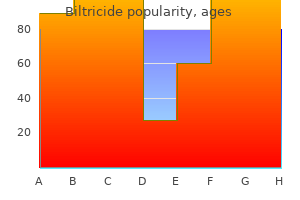
In recent years mueller sports medicine buy biltricide 600 mg on line, more than 90% of international adoptees are from Asian (China treatment without admission is known as purchase 600 mg biltricide visa, South Korea treatment carpal tunnel purchase biltricide 600 mg visa, Vietnam symptoms constipation purchase biltricide 600 mg mastercard, India treatment pink eye discount 600mg biltricide mastercard, Kazakhstan world medicine order 600 mg biltricide, and Philippines), Latin American and Caribbean (Guatemala, Colombia, and Haiti), Eastern European (Russia and the Ukraine), and African (Ethiopia, Nigeria, Liberia, and Ghana) countries. The diverse birth countries of these children, their unknown medical histories before adoption, their previous living circumstances (eg, orphanages and/or foster care), and the limited availability of reliable health care in some resource-limited countries make the medical evaluation of internationally adopted children a challenging but important task. Internationally adopted children typically differ from refugee children in terms of their access to medical care and treatment before arrival in the United States and in the frequency of certain infectious diseases. Many refugee children may have resided in refugee camps for months before resettlement in the United States and will have had access to limited medical care and treatment services. The history of access to and quality of medical care for international adoptees can be variable. However, this examination is limited to completing legal requirements for screening for certain communicable diseases and examination for serious physical or mental defects that would prevent the issue of an immigrant visa. During preadoption visits, pediatricians can stress to prospective parents the importance of acquiring immunization and other health records. Internationally adopted children who are 10 years of age and younger may obtain a waiver of exemption from the Immigration and Nationality Act regulations pertaining to immunization of immigrants before arrival in the United States (see Refugees and Immigrants, p 101). Children adopted from countries that are not part of the Hague Convention can receive waivers to have their immunizations delayed until arrival in the United States ( However, the child should be seen by his or her pediatrician or a physician 1 For additional information, see Canadian Paediatric Society. Infectious diseases are among the most common medical diagnoses identifed in international adoptees after arrival in the United States. Children may be asymptomatic, and therefore, the diagnoses must be made by screening tests in addition to history and physical examination. In addition to these infectious disease screening tests, other medical and developmental issues, including hearing and vision assessment, evaluation of growth and development, nutritional assessment, blood lead concentration, complete blood cell count with red blood cell indices and differential of white blood cells Table 2. Parents who have not met with a physician before adoption should notify their physician when their child arrives so that a timely medical evaluation can be arranged. Internationally adopted children should be examined as soon as possible after arrival in the United States, preferably within the frst 2 weeks after arrival. A list of pediatricians with special interest in adoption and foster care medicine is available on the American Academy of Pediatrics Web site at 2. Over the past 5 to 10 years, the number of countries with routine infant hepatitis B immunization programs has increased markedly. However, administration of a birth dose of hepatitis B vaccine, needed to prevent perinatal transmission from an infected mother, is not routine in many countries, and coverage among infants can be suboptimal. Although hepatitis B serologic tests are performed routinely in the country of origin, testing may be incomplete and children may become infected after testing. Serologic testing for acute infection (hepatitis A IgM) and immunity (total hepatitis A antibody) can be performed at the initial visit to determine whether the child has a current hepatitis A infection or immunity. In addition, hepatitis A vaccine should be administered to all susceptible nontraveling people who anticipate having close personal contact with a child adopted internationally from a country with high or intermediate hepatitis A endemicity before arrival of the adoptee. Adopted children or their household or other close contacts with symptoms consistent with acute viral hepatitis should be evaluated promptly. Children without hepatitis A immunity who are 12 months of age and older should receive hepatitis A vaccine as recommended according to the routine immunization schedule 1. Intestinal Pathogens Fecal examinations for ova and parasites by an experienced laboratory will identify a pathogen in 15% to 35% of internationally adopted children. The prevalence of intestinal parasites varies by age of the child and country of origin. The most common pathogens identifed are Giardia intestinalis, Dientamoeba fragilis, Hymenolepis species, Ascaris lumbricoides, and Trichuris trichiura. Strongyloides stercoralis, Entamoeba histolytica, and hookworm are recovered less commonly. Therapy for intestinal parasites generally will be successful, but complete eradication may not occur. Therefore, repeat ova and parasite testing after treatment is important to ensure successful elimination of parasites if symptoms persist. Children who fail to demonstrate adequate catch-up growth, who have unexplained anemia, or who have gastro intestinal tract symptoms or signs that occur or recur months or even years after arrival in the United States should be reevaluated for intestinal parasites. Tuberculosis Latent tuberculosis infection commonly is encountered in international adoptees from all countries, although incidence rates of tuberculosis vary by country. All immigrants, including international adoptees, are required to have screening for tuberculosis before arriving in the United States. Information about the screening and implementation requirements is available at However, some international adoptees may be anergic because of malnutrition, which is common in malnourished children. In these children, further investigation is necessary to determine whether latent tuberculosis infection or active disease is present and therapy is needed (see Tuberculosis, p 736). Some children will have had recent exposure to a person with tuberculosis disease. When active tuberculosis is suspected in an international adoptee, efforts to isolate and test the organism for drug susceptibilities are imperative because of the high prevalence of drug resistance in many countries. Syphilis Congenital syphilis, especially with involvement of the central nervous system, may not have been diagnosed or may have been treated inadequately in adoptees from some resource-limited countries. Children 15 years of age and older should have had serologic testing for syphilis as part of the required overseas medical assessment. Children who had positive test results are required to complete treatment before arrival in the United States. Children with positive treponemal serologic test results should be evaluated by a health care professional with special expertise to assess the differential diagnosis of pinta, yaws, and syphilis and to determine extent of infection so appropriate treatment can be administered (see Syphilis, p 690). Transplacentally acquired maternal antibody in the absence of infection can be detected in a child younger than 18 months of age. Chagas Disease (American Trypanosomiasis) Chagas disease is endemic throughout much of Mexico and Central and South America (see American Trypanosomiasis, p 734). Although the risk of Chagas disease is low in internationally adopted children from countries with endemic infection, treatment of infected children is highly effective. Countries with endemic Chagas disease include Argentina, Belize, Bolivia, Brazil, Chile, Colombia, Costa Rica, Ecuador, El Salvador, French Guiana, Guatemala, Guyana, Honduras, Mexico, Nicaragua, Panama, Paraguay, Peru, Suriname, Uruguay, and Venezuela. Transmission within countries with endemic infection is focal, but if a child comes from a country with endemic Chagas disease, testing for Trypanosoma cruzi should be considered. Serologic testing should be performed only in children 12 months of age or older because of the potential presence of maternal antibody. Other Infectious Diseases Skin infections that occur commonly in international adoptees include bacterial (eg, impetigo) and fungal (eg, candidiasis) infections and ectoparasitic infestations (eg, scabies and pediculosis). Diseases such as typhoid fever, malaria, leprosy, or melioidosis are encountered infrequently in internationally adopted children. If the child came from a country where malaria is present, malaria should be considered in the differential diagnosis (see Malaria, p 483). In 2002 and 2004, adoptions from affected orphanages were suspended temporarily while Chinese authorities implemented measures to control and prevent further transmission of measles among the children. Measles elimination has been achieved only in the Americas; transmission continues in other parts of the world. In 2011, measles importation into the United States occurred from more than 22 countries, but because of high immunization rates, secondary cases were minimal. All people born after 1957 should receive 2 doses of measles-containing vaccine in the absence of documented measles infection or contraindication to the vaccine (see Measles, p 489). Clinicians should be aware of potential diseases in internationally adopted children and their clinical manifestations. Some diseases, such as central nervous system cysticercosis, may have incubation periods as long as several years and, thus, may not be detected during initial screening. On the basis of fndings at the initial evaluation, consideration should be given to a repeat evaluation 6 months after adoption. In most cases, the longer the interval from adoption to development of a clinical syndrome, the less likely the syndrome can be attributed to a pathogen acquired in the country of origin. In international adoptees who have negative stool ova and parasite test results and in whom eosinophilia (absolute eosinophil count exceeding 450 cells/mm) is found 3 on review of complete blood cell count, serologic testing for strongyloidiasis, schistosomiasis, and lymphatic flariasis should be considered. Serologic testing for Strongyloides stercoralis should be performed on all international adoptees with eosinophilia and no identifed pathogen commonly associated with an increased eosinophil count, regardless of country of origin. Serologic testing for Schistosoma species should be performed on international adoptees with eosinophilia and no identifed pathogen commonly associated with eosinophilia who are from Sub-Saharan Africa, South East Asia, or areas of Latin America where schistosomiasis is endemic. Serologic testing for lymphatic flariasis should be considered in international adoptees older than 2 years of age with eosinophilia who are from countries with endemic lymphatic flariasis ( Immunizations Only written documentation of immunizations received by an adoptee should be accepted. However, because other immunizations such as Haemophilus infuenzae type b, Streptococcus pneumoniae, mumps, rubella, hepatitis A, and varicella vaccines are given less frequently or are not part of the routine immunization schedule in other countries, written documentation may be available less often. Although some vaccines with inadequate potency are used in other countries, most vaccines available worldwide are produced with adequate quality-control standards and are reliable. However, information about storage, handling, site of administration, vaccine potency, and provider generally is not available. Given the limited data available regarding verifcation of immunization records from other countries, evaluation of concentrations of antibody to the antigens given repeatedly is an option to ensure that vaccines were given and were immunogenic. Serologic testing may be performed to determine whether protective antibody concentrations are present. In children older than 6 months of age with or without written documentation of immunization, serologic testing for antibodies to diphtheria and tetanus toxoids and poliovirus may be considered to determine whether the child has protective antibody concentrations. In children older than 12 months of age, hepatitis A, measles, mumps, rubella, and varicella antibody concentrations may be measured to determine whether the child is immune; these antibody tests should not be performed in children younger than 12 months of age because of the potential presence of maternal antibody. At this time, no antibody testing is reliable or available routinely to assess immunity to pertussis. If serologic testing is not available and receipt of immunogenic vaccines cannot be ensured, the prudent course is to provide the immunization series. Even if the potential for the discarded syringe to contain a specifc bloodborne pathogen can be estimated from the background prevalence rates of these infections in the local community, the need to test the injured or exposed person usually is not infuenced signifcantly by this assessment. Wound Care and Tetanus Prophylaxis Management of people with needlestick injuries includes acute wound care and consideration of the need for antimicrobial prophylaxis. Standard wound cleansing and care is indicated; such wounds rarely require closure. Tetanus toxoid vaccine, with or without Tetanus Immune Globulin, should be considered as appropriate for the age, the severity of the injury, the immunization status of the exposed person, and the potential for dirt or soil contamination of the needle (see Tetanus, p 707). The preferred tetanus toxoid vaccine is tetanus and diphtheria toxoids and reduced acellular pertussis (Tdap; see Pertussis, p 553), but tetanus and diphtheria toxoids (Td) vaccine should be used if the patient has already received Tdap at some point in the past, because current recommendations are for only a single administration of Tdap. Risk of acquisition of various pathogens depends on the nature of the wound, the ability of the pathogens to survive on environmental surfaces, the volume of source material, the concentration of virus in the source material, prevalence rates among local injection drug users, the probability that the syringe and needle were used by a local injection drug user, and the immunization status of the exposed person. Pediatric injuries from needles discarded in the community: epidemiology and risk of seroconversion. Administration of Hepatitis B Immune Globulin usually is not indicated if the child has received the 3-dose regimen of hepatithis B vaccine. If the child has received 2 doses of hepatitis B vaccine 4 or more months previously, the immediate administration of the third dose of vaccine alone should be suffcient in most cases. Experts differ in opinion about the need for Hepatitis B Immune Globulin at the time of an injury of an incompletely immunized child. Negative results from these initial tests support the conclusion that any subsequent positive test result likely refects infection acquired from the needlestick. A positive initial test result in a pediatric patient requires further investigation of the cause, such as perinatal transmission, sexual abuse or activity, or drug use. Counseling is necessary before and after testing (see Human Immunodefciency Virus Infection, p 418). Antiretroviral therapy is not without risk and often is associated with signifcant adverse effects (see Human Immunodefciency Virus Infection, p 418). If the decision to begin prophylaxis is made, any delay before starting the medications should be minimized (see Human Immunodefciency Virus Infection, p 418). Medication should begin within 72 hours and should continue for 28 days in combination of 2 or 3 antiretroviral drugs. Although transmission by sharing syringes among injection drug users is effcient, the risk of transmission from a discarded syringe is likely to be low. Positive test results should be confrmed by supplemental confrmatory laboratory tests (see Hepatitis 1 Centers for Disease Control and Prevention. Preventing Needlestick Injuries Needlestick injuries of both children and adults can be minimized by implementing public health programs on safe needle disposal and programs for exchange of used syringes and needles from injection drug users for sterile needles. Syringe and needle exchanges decrease improper disposal and spread of bloodborne pathogens without increasing the rate of injection drug use. The American Academy of Pediatrics supports needle-exchange programs in conjunction with drug treatment and within the context of continuing research to assess their effectiveness. Bite Wounds As many as 1% of all pediatric visits to emergency departments during summer months are for treatment of human or animal bite wounds. An estimated 5 million bites occur annually in the United States; dog bites account for approximately 90% of those wounds. The rate of infection after cat bites is as high as 50%; rates of infection after dog or human bites are 10% to 15%.
The presence or absence of antibody should not be used to initiate or terminate therapy medications you cant donate blood discount biltricide american express, because antibody is not demonstrable in a few patients with the disease and may be present in patients without active disease symptoms hepatitis c biltricide 600 mg visa. Alveolar hemorrhage in anti-basement membrane antibody disease: a series of 28 cases treatment 7th feb cheap biltricide 600 mg. Clinical and morphological aspects of the managebrane antibody disease: analysis of prognostic significance of ment of crescentic anti-glomerular basement membrane antibody clinical medicine 512 discount biltricide 600 mg without a prescription, pathologic and treatment factors medicine kidney stones buy generic biltricide 600 mg line. Patients present with bleeding and bruising (most common) medications mothers milk thomas hale buy discount biltricide 600mg on-line, along with anemia and/or infection. Diagnosis and manageReferences of the identified articles were searched for additional ment of acquired pure red cell aplasia. In parallel, decreased skin infiltration by inflammatory cells and improved skin architecture were observed. Double-filtration apy, and plasma exchange and plasmapheresis for articles published plasmapheresis for the treatment of patientswith recalcitrant in the English language. Knobler R, Berlin G, Calzavara-Pinton P, Greinix H, Jaksch P, Laroche L, Ludvigsson J, Quaglino P, Reinisch W, Scarisbrick J, 1. Apheresis in the treatment of recalcitrant atopic derBohbot A, Bruckner-Tuderman L, Dreno B, Enk A, French L, matitis: case series and review of the literature. Philadelphia: ElsevImprovement of treatment-refractory atopic dermatitis by immuier. It is typically seen in the post-infectious setting (as polyclonal autoantibodies) or in lymphoproliferative disorders (as monoclonal autoantibodies). The thermal amplitude is defined as the highest temperature at which the antibody reacts with its cognate antigen. Rituximab is another second-line therapy with documented short-term efficacy, and limited information on long-term efficacy. In patients who have severe disease, the most effective and best-evaluated treatment is rituximab in the standard lymphoma dose and is now recommended first-line therapy, although complete and sustained remissions are uncommon. How I treat autoimmune hemolytic anemias searched for additional cases and trials. A case report of tive analysis of 30 severe autoimmune hemolytic anemia refractory warm autoimmune hemolytic anemia treated with plaspatients treated by whole blood exchange transfusion. Autoimmune pathogenesis and autoplasma exchange: a case report and review of the literature. Excessive cytokine production is thought to be a major cause of severe babesiosis and is associated with tissue pathology that can lead to significant end-organ damage and can result in persistent relapsing disease or death (all-cause mortality <1% of clinical cases and about 10% in transfusion transmitted cases). The detection of IgM is indicative of recent infection while IgG titer of 1:1,024 or greater usually signify active or recent infection. Combination of quinine sulfate and clindamycin is equally effective but associated with more adverse reactions. Decreased myocardial contractility and inappropriate cardiac output may produce hemodynamic fragility. Is there a role for plasmapheresis/exchange transfusion in the treatment of the septic burn patientfi Effect of plasma the effect of plasma exchange on lymphocyte suppression after exchange therapy on circulating fibronectin in burned patients. Resources for Optimal Care of the Gibbons L, Holavanahalli R, Hunt C, Keller K, Kirk E, Laird J, Burn Patient. The beneficial effects of plasma exchange after Plasma exchange therapy in patients failing to resuscitate from severe burn injury. Forty-one percent (41%) of neonates have at least one other affected sibling; there is a 17% chance of recurrence in subsequent pregnancies. This group used a similar regimen for 2 previous (successful reversion of 2nd degree) and 4 future (no reversion of 2nd or 3rd degree) pregnancies. A combination therapy protocol of plasmapheresis, intraverence and therapeutic approach to prevention. Di Mauro A, Caroli Casavola V, Favia Guarnieri G, Calderoni L, Gerosa M, Mosca M, Ghirardello A, Tani C, Motta M, G, Cicinelli E, Laforgia N. Successful preventive cardiac disease: a scientific statement from the American Heart treatment of congenital heart block during pregnancy in a Association. A consensus conference report on the sensitized patient awaiting heart transplantation discusses several aspects of this process (Colvin, 2015). Apheresis techniques have helped to avoid the intensive use of immunosuppressives and provide adjunctive therapy in desensitization and rejection protocols. Treatments are typically continued until improvement/stabilization of symptoms occurs. Outcomes in highly sensitized pediatric heart transplant with hemodynamic compromise: objective evidence for efficacy patients using current management strategies. Photopheresis for the prevention of rejection in strategy to shorten left ventricular assist device support. Rapid reduction in donor-specific antidiology; American Heart Association Heart Failure and Transhuman leukocyte antigen antibodies and reversal of antibodyplantation Committee of the Council on Cardiopulmonary mediated rejection with bortezomib in pediatric heart transplant Critical Care, Perioperative and Resuscitation; American Heart patients. Reduction of alloantibodies via proteasome inhibition in carHeart Association Heart Failure and Transplantation Committee diac transplantation. Therapeutic apheresis in transantibody-mediated rejection in heart transplantation. Anticoagulation with heparin serves to both inhibit clot generation and promote clot fibrinolysis. The role of rituximab and eculizimab, particularly for relapse prevention, remains unclear and research is ongoing. Technical notes Plasma as the replacement fluid repletes natural anticoagulants such as antithrombin and proteins C and S. Since plasma antithrombin is essential to mediate anticoagulation with heparin, the use of albumin alone as replacement fluid may prevent the beneficial effect of heparin unless levels of antithrombin are serially monitored and heparin anticoagulation is adequate by laboratory monitoring. Cervera R, Rodrfiguez-Pinto I, Colafrancesco S, Conti F, Valesini G, Rosario C, Agmon-Levin N, Shoenfeld Y, Ferrao~ C, As of November 3, 2015, using PubMed and journals published in Faria R, Vasconcelos C, Signorelli F, Espinosa G. The hallmarks of the syndrome are intractable focal seizures resistant to anticonvulsant drugs, progressive unilateral cerebral atrophy leading to progressive hemiparesis, loss of function in the affected cerebral hemisphere, and cognitive decline. Current management/treatment Treatment aims to reduce seizure activity and frequency and improve the functional long-term outcome, as measured by both motor and cognitive performance. Subtotal, functionally complete hemispherectomy may markedly reduce seizure activity in a majority of patients but results in permanent contralateral hemiplegia. In general, immunotherapy slows disease progression but none has halted nor cured the disease. More recent reports indicate that Serum GluR3 immunoreactivity, which was found in only few patients with Rasmussen encephalitis, is a feature of epilepsy syndromes and not specific to Rasmussen encephalitis. A similar approach may be taken in subsequent courses if a salutary clinical effect is apparent. Focal seizures due to chronic localized encephB-lymphocytes in Rasmussen encephalitis. Similar clinical presentations may be seen with inherited, paraneoplastic and toxic neuropathies, and neuropathies associated with nutritional deficiency, porphyria, or critical illness. Therapies should be initiated early to stop the inflammatory demyelination and prevent secondary axonal degeneration, and therefore permanent disability. Therapeutic response is measured by improvement or stabilization of neurological symptoms, at which point treatment can be tapered or discontinued. Beppu M, Sawai S, Misawa S, Sogawa K, Mori M, Ishige T, patients with neurological diseases: multicenter retrospective Satoh M, Nomura F, Kuwabara S. Plasma exchange in chronic inflammatory demyelinatpolyneuropathy: a five year follow up of 38 cases. Monoclonal proteins may also bind to coagulation factors leading to acquired deficiency or functional defects (laboratory assays of coagulation function may not accurately reflect the hemostatic derangement and bleeding risk). Bleeding tendency with factor inhibitors is due to clearance of the specific factor and/or direct inhibition of the factor function. Polyclonal sheep antibodies bind all classes of Ig causing a large decrease in IgG levels. Sugiyama H, Uesugi H, Suzuki S, Tanaka K, Souri M, Ichinose tein A immunoadsorption. Ambaglio C, Lodo F, Trinchero A, Ghidelli N, Perotti C, Del high-risk haemorrhagic surgery. Jansen M, Schmaldienst S, Banyai S, Quehenberger P, Pabinger life-threatening lower limb haemorrhage. Patients can also have systemic symptoms involving organ systems, including respiratory, cardiovascular (tachycardia, orthostatic intolerance), gastrointestinal (dysmotility), genitourinary (urinary retention), weakness, fatigue, and others. Many therapeutic agents have been used with variable and often partial effects including bisphosphonates, gabapentin, calcitonin, intravenous ketamine, free radical scavengers, oral corticosteroids, and spinal cord stimulation. Longstanding complex regional pain syndrome is assoComplex Regional Pain Syndrome and plasma exchange, plasmaciated with activating autoantibodies against alpha-1a adrenoceppheresis or apheresis for reports published in the English language. The aggregates of cryoglobulins can deposit on small vessels and cause damage by activating complement and recruiting leukocytes. This most commonly occurs on the skin of lower extremities because of exposure to lower temperatures. When cryoglobulinemic vasculitis is present, the disease is referred to as CryoVas. The diagnosis of cryoglobulinemia is made by history, physical findings, low complement levels, and detection and characterization of cryoglobulins (including quantitation by the cryocrit). A large case series (CryoVas survey) demonstrated greatest therapeutic efficacy of rituximab plus corticosteroids over corticosteroids alone or with alkylating agents in patients with noninfectious mixed CryoVas. It has been used mostly in active moderate to severe cryoglobulinemia with renal impairment (membranoproliferative glomerulonephritis), neuropathy, arthralgia, and/or ulcerating purpura. Double or cascade filtration, which separates plasma out of whole blood in the first filter and removes high molecular weight proteins in the second filter (such as IgM), has also been used to treat cryoglobulinemia. Another apheresis modality used in this disease is cryofiltration or cryoglobulinapheresis, which cools the plasma in an extracorporeal circuit either continuously or in a two step procedure to remove cryoglobulins, the remaining plasma is warmed to body temperature prior to returning to the patient. Referenofiltration apheresis for treatment of cryoglobulinemia associces of the identified articles were searched for additional cases and ated with hepatitis C. Terrier B, Krastinova E, Marie I, Launay D, Lacraz A, Cryoglobulinemia Vasculitis. Terrier B, Marie I, Lacraz A, Belenotti P, Bonnet F, Chiche L, Miglairesi S, Galli M, Bombardieri S, MontiG. Apheresis in cryoglobulinemia compliculitis: results from the French nationwide CryoVas survey and cating hepatitis C and in other renal diseases. Urraro T, Gragnani L, Piluso A, Fabbrizzi A, Monti M, Fognani bulinemia: updates on clinical features and treatment advances. Patients should be monitored and responses documented as per published guidelines. Extracorporeal photopheresis for the treatment the European Organisation for Research and Treatment of Canof Sezary syndrome using a novel treatment protocol. Primary cutaneous T-cell lymphoma (mycosis fungoides and for therapy by the United States Cutaneous Lymphoma ConsorSezary syndrome). Knobler R, Berlin G, Calzavara-Pinton P, Greinix H, Jaksch P, goides and Sezary syndrome. High clinical response rate of Sezary L, Gniadecki R, Gollnick H, Hertl M, Jantschitsch C, Jung A, syndrome to immunomodulatory therapies.
She associated skin eruption that occurred in annulare was counseled on the diagnosis and his early childhood treatment kidney stones buy discount biltricide 600 mg on-line. Why such ostensibly diverse oral and intramuscular glucocorticoid profile treatment abbreviation cheap biltricide american express, with increased or decreased white clinical and pathophysiological entities as 15 16 therapy seems to be the treatment of cell count medications via g-tube order biltricide online now, lymphocytosis or lymphopenia medicine 93 3109 buy discount biltricide line, acute renal failure medicine 3605 v buy 600 mg biltricide with amex, hypothyiroidism treatment 5 of chemo was tuff but made it purchase generic biltricide line, 1 17 choice in the clinical management of the and thrombocytosis or thrombocytopenia. Systemic antihistamines with topical Skin eruptions typically resolve completely reportedly induced cases of acute febrile steroids may also be of some value as well over time; nevertheless, some residual postneutrophilic dermatosis remains a medical as yield symptomatic resolution. Antibiotic therapy is the more often than men (female predominance pathways yet converging end results. Eruption is comprised of relationship between the ingestion of Anecdotal alternative treatments exist, painful papules, pustules, or nodules the offending drug and the onset of with select case reports pointing to their forming sharply demarcated inflammatory cutaneous outbreaks. Potassium iodide, oral plaques with intense edematous reaction is an expected remediation of symptoms 37 38 39 metronidazole, dapsone, colchicine, reminiscent of vesiculation. Jeanfils S, Joly P, Young P, Le Corvaisier-Pieto C, chronic lymphocytic leukemia associated with neutropenic Thomine E, Lauret P. Rodriguez de la Serna A, Domingo-Pedrol P, BlanchTorra L, Perez-Perez A, Obrador-Mayol D. Sweet syndrome following therapeutic use of granulocyte colony stimulating factor. Fukutoku M, Shimizu S, Ogawa Y, Takeshita S, Masaki Y, Arai T, Hirose Y, Sugai S, Konda S, Takiguchi T. In clinical trials, the most common adverse events reported were gastrointestinal upsets, nasopharyngitis/pain and nasal congestion/sinusitis. All contraindications, warnings and precautions associated with tetracyclines must be considered before prescribing Oracea. The cost for this advertising is: Black and White 1/4 page-$125, 1/2 page-$200, full page-$350 Full 4 color ad 1/4 page-$275, 1/2 page-$350, full page-$500 Resident members may run a 3" column black and white ad stating their desired professional position. However, this age is not a firm reference point because some of the recommended regimens have not been comprehensively tested across all ages. The recommended dose of radiation, where given, is highly dependent on the intensity of systemic chemotherapy; thus, it is critical to adhere to a given treatment protocol in its entirety. Leucovorin remains a component in the treatment of methotrexate toxicity and should be continued for at least 2 days following glucarpidase administration. However, this age is not a frm reference point because some of the recommended regimens have not been comprehensively tested across all ages. The evaluated on an individual basis, including for the following factors: end-organ optimal duration is unknown. All regimens include induction/ lChronological age is a poor surrogate for fitness for therapy. Patients should be delayed intensification (especially for pediatric-inspired regimens) and evaluated on an individual basis, including for the following factors: end-organ maintenance therapy. All regimens include induction/delayed intensification (especially for pediatric-inspired regimens) and maintenance therapy. Patients should be evaluated on an individual basis, including for the following factors: end-organ reserve, end-organ dysfunction, and performance status. However, be aware that leucovorin is a substrate for glucarpidase, and therefore should not be administered within two hours prior to or following glucarpidase. The toxicity profile of both asparaginase products presents significant challenges in clinical management. Prevention and management of asparaginase/pegasparaginaseassociated toxicities in adults and older adolescents: recommendations of an expert panel. Of particular concern are Grade 2 or higher systemic allergic reactions, urticaria, or anaphylaxis, because these episodes can be (but are not necessarily) associated with neutralizing antibodies and lack of efficacy. In the case of Grade 2 pancreatitis (enzyme elevation or radiologic findings only), asparaginase should be held until these findings normalize and then resume. Clinical application of asparaginase activity levels following treatment with pegaspargase. Upon resolution of symptoms and antithrombotic therapy stable or completed, consider resuming asparaginase. For Grade 3 or less, if symptoms/signs fully resolve, consider resuming asparaginase at lower doses and/or longer intervals between doses. For Grade 3 or higher, hold asparaginase and steroids until blood glucose has been regulated with insulin, then resume. It may be necessary to reduce dose/eliminate antimetabolite in the setting of myelosuppression and/or hepatotoxicity. However, it is associated with a high frequency of serious vascular events (eg, strokes, heart attacks, tissue ischemia). It is important that the instruction for blinatumomab product preparation (including admixing) and administration are strictly followed to minimize medication errors, including underdose and overdose. Improved early event-free survival with imatinib in Philadelphia chromosome23Linker C, Damon L, Ries C, Navarro W. Am J Hematol Mesylate Regimen for Adults with De Novo or Minimally Treated Philadelphia Chromosome (Ph) Positive Acute 2010;85:164-170. Pre-transplant imatinib-based therapy improves the outcome of allogeneic 31Kantarjian H, Giles F, Wunderle L, et al. Nilotinib combined with multiagent chemotherapy for newly diagnosed Philadelphia33Martinelli G, Boissel N, Chevallier P, et al. Complete hematologic and molecular response in adult patients with positive acute lymphoblastic leukemia. Dasatinib and low intensity chemotherapy for first-line treatment in patients 37Kantarjian H, Stein A, Gokbuget N, et al. Blood 2015;126:964-971 T-lineage acute lymphoblastic leukemia or lymphoblastic lymphoma: Cancer and Leukemia Group B study 19801. Safe integration of nelarabine into intensive chemotherapy in newly Blood 2007;109:5136-5142. Clin Lymphoma Myeloma regimen in adults with untreated acute lymphoblastic leukemia [abstract]. Comparison of the results of the treatment of adolescents and young adults with chromosome negative acute lymphoblastic leukemia [abstract]. Pharmacokinetics-based integration of multiple doses of intravenous resistant acute leukemia in pediatric patients. For those patients with advanced age, multiple comorbidities, and/or poor functional status, lower dose chemotherapy consisting of vincristine and steroids have efectively been used for decades. For instance, asparaginase has been removed from induction, and anthracycline doses have been reduced by 50% or omitted in some regimens. For appropriate ft individuals achieving remission, consideration of autologous or reduced-intensity allogeneic stem cell transplantation may be appropriate. Dasatinib and low-intensity chemotherapy in elderly vincristine, doxorubicin and dexamethasone in elderly patients with acute lymphocytic leukemia. Abdominal masses from 11, 2015 and November 18, 2016, using the following search term: gastrointestinal involvement, or chin numbness resulting from cranial acute lymphoblastic leukemia. Fertility counseling and preservation options should be presented to all patients. Early marrow response to therapy was a strong positive disease, and response to induction therapy have been identified as prognostic factor while the presence of extramedullary disease at important factors in defining risk and assessing prognosis for both adult diagnosis was correlated with a poorer prognosis. Compared to the pediatric encompassing 27%, 32%, 27%, and 4% of cases, respectively. Furthermore, the positive prognostic improved survival outcomes for these patients. Thus, the choice of initial treatment regimen can have a parental supervision of the treatment and better insurance. In general, the treatment phases can be largely grouped into and dexamethasone was associated with a significantly higher risk of induction, consolidation, and maintenance. Additionally, histamine-2 antagonist or proton pump inhibitors can affect the and 36%, respectively. The efficacy and safety of chemotherapy versus those who received chemotherapy alone (72. At with dasatinib combined with low-intensity chemotherapy (vincristine a median follow-up of 1. Although no the previous study was not designed as a randomized controlled trial, randomized controlled trials have yet been conducted to establish the and the number of patients in the non-imatinib group was small. A panel of experts from the European LeukemiaNet included diarrhea (74%), nausea (48%) and vomiting (44%). Some investigators have reported on the feasibility of serious cardiovascular adverse events. Individuals who inherit a nonfunctional variant allele treated in a clinical trial, when possible. As regimen, as tolerated; however, the doses of antimetabolites may need previously mentioned, although the optimal duration of post-transplant to be reduced in the setting of hepatotoxicity or myelosuppression. Dexamethasone showed improved therapy as either slow early responders (patients with >25% bone outcomes during induction patients in younger than 10 years of age; marrow blasts on day 7 of induction) or rapid early responders. Among however, it was associated with a higher risk of osteonecrosis in the patients who were rapid early responders to induction (n = 1299), patients 10 years of age or older. These data suggest that age may be the augmented postinduction intensity arm was associated with an important factor for the selection of a corticosteroid. These initial safety data suggest that treatment protocol includes a 4-drug induction regimen with intrathecal nelarabine may be better tolerated in frontline regimens than in the cytarabine and intrathecal methotrexate, consolidation, interim relapsed/refractory setting. Among patients with standard no significant advantage was observed in a donor versus no-donor risk, the non-relapse mortality rate at 2 years was 19. A subgroup analysis showed a significant survival poor prognostic factor and 97 (57%) had multiple risk factors. All other Ph-negative patients were median time to platelet recovery in patients fi60 years (placebo group, 26 days vs. Remission rates within 12 weeks after treatment a second or greater bone marrow relapse (n = 36). The 30-day mortality rate was 9% and median remission Clofarabine is a nucleoside analog approved for the treatment of duration was 5 months. For fit patients, additional therapy may (regardless of risk group) be treated in a clinical trial, where possible. Multiagent relapses (ie, relapses occurring fi36 months from initial diagnosis), rechemotherapy protocols based on data from single-institution studies, treatment with the same induction regimen is a reasonable option. Dose modifications may be For relatively fit patients (age <65 years without substantial required for chemotherapy agents, as needed. Chemotherapy should be initiated as soon as possible; combination chemotherapy has shown improved response though relapse is For recommendations on the treatment of adult patients with mature B293 common. For late doxorubicin, and dexamethasone alternating with cycles of high-dose relapses (ie, relapses occurring fi36 months from initial diagnosis), remethotrexate and cytarabine) is also a common regimen used for treatment with the same induction regimen is a reasonable option. A response rate of 100% was seen in a other patients, participation in a clinical trial is preferred, when possible. In this study, patients were use of irradiation can be reserved for advanced disease. A testicular examination should be performed for all male patients at Pediatric-inspired treatment regimens typically include lumbar puncture diagnostic workup; testicular involvement is especially common among at diagnostic workup. Patients with clinical evidence of testicular performed, be conducted concomitantly with initial intrathecal therapy. Radiation therapy is typically performed concurrently with the first incorporates methotrexate. Relapsed leukemia at diagnosis should receive adequate systemic therapy as Version 5. During the first year after completion of therapy, 10 30,305 bone marrow: up to 10 malignant cells.
In addition to fever symptoms gastritis 600 mg biltricide amex, children with K kingae bacteremia frequently have concurrent fndings of respiratory or gastrointestinal tract disease medications bladder infections order biltricide 600mg visa. Of the 4 species in the genus Kingella medications cause erectile dysfunction biltricide 600 mg on-line, K kingae is the species most commonly associated with infection medicine used for pink eye 600mg biltricide overnight delivery. The organism more frequently colonizes young children than adults and can be transmitted among children in child care centers symptoms 6 days dpo generic biltricide 600 mg mastercard, generally without causing disease symptoms vomiting diarrhea buy biltricide 600mg lowest price. Infection may be associated with preceding or concomitant stomatitis or upper respiratory tract illness. In patients with pyogenic arthritis and osteomyelitis, blood cultures often are negative for K kingae. Synovial fuid and bone aspirates from patients with suspected K kingae infection should be inoculated into Bactec, BacT/ Alert, or similar blood culture systems and held for at least 7 days to maximize recovery. Conventional and real-time polymerase chain reaction methods have improved detection of K kingae in research studies. K kingae should be suspected in young children with culturenegative skeletal infections. Strains generally are susceptible to ampicillin-sulbactam, aminoglycosides, ciprofoxacin, erythromycin, chloramphenicol, and oxacillin and are resistant to trimethoprim, clindamycin, and vancomycin. Gentamicin in combination with penicillin can be useful for the initial treatment of endocarditis. Extendedspectrum cephalosporins cefotaxime or ceftriaxone also may be used to treat endocarditis. Legionnaires disease varies in severity from mild to severe pneumonia characterized by fever, cough, and progressive respiratory distress. Legionnaires disease can be associated with chills, myalgia, gastrointestinal tract, central nervous system, and renal manifestations. Pontiac fever is a milder febrile illness without pneumonia that occurs in epidemics and is characterized by an abrupt onset and a self-limited, infuenzalike illness. At least 20 different species have been implicated in human disease, but the most common species causing infections in the United States is Legionella pneumophila, with most isolates belonging to serogroup 1. More than 80% of cases are sporadic; the sources of infection can be related to exposure to L pneumophila-contaminated water in the home, workplace, or hospitals or other medical facilities or to aerosol-producing devices in public places. Outbreaks have been ascribed to common-source exposure to contaminated cooling towers, evaporative condensers, potable water systems, whirlpool spas, humidifers, and respiratory therapy equipment. Outbreaks have occurred in hospitals, hotels, and other large buildings as well as on cruise ships. Health care-associated infections can occur and often are related to contamination of the hot water supply. Legionnaires disease occurs most commonly in people who are elderly, are immunocompromised, or have underlying lung disease. Infection in children is rare and usually is asymptomatic or mild and unrecognized. Severe disease has occurred in children with malignant neoplasms, severe combined immunodefciency, chronic granulomatous disease, organ transplantation, end-stage renal disease, underlying pulmonary disease, and immunosuppression; in children receiving systemic corticosteroids; and as a health care-associated infection in newborn infants. The incubation period for Legionnaires disease (pneumonia) is 2 to 10 days; for Pontiac fever, the incubation period is 1 to 2 days. Detection of Legionella antigen in urine by commercially available immunoassays is highly specifc. Such tests are sensitive for L pneumophila serogroup 1, but these tests rarely detect antigen in patients infected with other L pneumophila serogroups or other Legionella species. Convalescent serum samples should be obtained 3 to 4 weeks after onset of symptoms; however, a titer increase can be delayed for 8 to 12 weeks. The positive predictive value of a single titer of 1:256 or greater is low and does not provide defnitive evidence of infection. Newer serologic assays, such as enzyme immunoassay or tests using Legionella antigens other than serogroup 1, are available commercially but have not been standardized adequately. Levofoxacin (or another fuoroquinolone) is the drug of choice for immunocompromised patients, because fuoroquinolone antimicrobial agents are bactericidal and are more effective than macrolides in vitro and in animal models of infection, and limited available observational study data in adults suggest that clinical improvement (resolution of fever and duration of hospitalization) is more rapid with a fuoroquinolone than with a macrolide/azalide. Fluoroquinolones are not approved for this indication in children younger than 18 years of age (see Fluoroquinolones, p 800). Doxycycline should not be used for pregnant women or for children younger than 8 years of age unless there are no other therapeutic options (see Tetracyclines, p 801). Duration of therapy is 5 to 10 days for azithromycin and 14 to 21 days for other drugs. Longer courses of therapy are recommended for patients who are immunocompromised or who have severe disease. Occurrence of even a single laboratory-confrmed health care-associated case of legionellosis warrants consideration of an epidemiologic and environmental investigation. Hospitals with transplantation programs (solid organ or hematopoietic stem cell) should maintain a high index of suspicion of legionellosis, use sterile water for the flling and terminal rinsing of nebulization devices, and consider performing periodic culturing for Legionella species in the potable water supply of the transplant unit. Long-term decontamination of the potable water supply usually requires installation of a permanent disinfection system. Ulcerative lesions may become dry and crusted or may develop a moist granulating base with an overlying exudate. Lesions can, however, persist as nodules or papules and may be single or multiple. Lesions commonly are located on exposed areas of the body (eg, face and extremities) and may be accompanied by satellite lesions, which appear as sporotrichoid-like nodules, and regional adenopathy. Clinical manifestations of Old World and New World (American) cutaneous leishmaniasis are similar. Spontaneous resolution of lesions may take weeks to years and usually results in a fat atrophic (cigarette paper) scar. Hematogenous mucocutaneous leishmaniasis (espundia) primarily is associated with the Viannia subspecies. Mucosal involvement can occur by extension of facial lesions attributable to other species. It may become evident clinically from months to years after the cutaneous lesions heal; sometimes mucosal and cutaneous lesions are noted simultaneously. In some patients, granulomatous ulceration and necrosis follows, leading to facial disfgurement, secondary infection, and mucosal perforation, which may occur months to years after the initial cutaneous lesion heals. After cutaneous inoculation of parasites by the sand fy vector, organisms spread throughout the mononuclear macrophage system to the spleen, liver, and bone marrow. The resulting clinical illness typically manifests as fever, anorexia, weight loss, splenomegaly, hepatomegaly, anemia, leukopenia, thrombocytopenia sometimes associated with hemorrhage, hypoalbuminemia, and hypergammaglobulinemia. Secondary gramnegative enteric infections and tuberculosis may occur as a result of suppression of the cell-mediated immune response. At the other end of the spectrum are patients who are minimally symptomatic but harbor viable parasites lifelong. Cutaneous leishmaniasis typically is caused by Old World species Leishmania tropica, Leishmania major, and Leishmania aethiopica and by New World species Leishmania mexicana, Leishmania amazonensis, Leishmania braziliensis, Leishmania panamensis, Leishmania guyanensis, and Leishmania peruviana. Visceral leishmaniasis is caused by Leishmania donovani and Leishmania infantum (Leishmania chagasi is synonymous). However, people with typical cutaneous leishmaniasis caused by these organisms rarely develop visceral leishmaniasis. However, the only proven reservoir of L donovani in the Indian subcontinent consists of infected humans, and transmission has a large anthroponotic component in East Africa as well. Transmission primarily is vectorborne through the bite of infected female phlebotomine sand fies. Leishmaniasis is endemic in 88 countries, from northern Argentina to southern Texas (not including Uruguay or Chile), in southern Europe, China and Central Asia, the Indian subcontinent, the Middle East, and Africa (particularly East and North Africa, with sporadic cases elsewhere) but not in Australia or Oceania. Overall, visceral leishmaniasis is found in focal areas of approximately 65 countries. The estimated annual number of new cases of cutaneous leishmaniasis is approximately 1. Approximately 90% of cases of mucosal leishmaniasis occur in 3 countries: Bolivia, Brazil, and Peru. Geographic distribution of cases evaluated in the developed world refects travel and immigration patterns. The number of cases has increased as a result of increased travel to areas with endemic infection; for example, with ecotourism activities in Central and South America and military activities in Iraq and Afghanistan, the number of imported cases within North America has increased. The incubation periods for the different forms of leishmaniasis range from several days to several years but usually are in the range of several weeks to 6 months. In cutaneous leishmaniasis, primary skin lesions typically appear several weeks after parasite inoculation. A common way of identifying the parasite is by microscopic identifcation of intracellular leishmanial organisms (amastigotes) on Wrightor Giemsa-stained smears or histologic sections of infected tissues. In cutaneous disease, tissue can be obtained by a 3-mm punch biopsy, by lesion scrapings, or by needle aspiration of the raised nonnecrotic edge of the lesion. In visceral leishmaniasis, the organisms can be identifed in the spleen and, less commonly, in bone marrow and the liver. The sensitivity is highest for splenic aspiration (approximately 95%), but so is the risk of hemorrhage or bowel perforation. In East Africa in patients with lymphadenopathy, the organisms also can be identifed in lymph nodes. Isolation of parasites (promastigotes) by culture of appropriate tissue specimens in specialized media may take days to several weeks but should be attempted when possible. Knowledge of the infecting species may affect prognosis and infuence treatment decisions. Investigational polymerase chain reaction assays are available at some reference laboratories. Serologic test results usually are positive in cases of visceral and mucosal leishmaniasis if the patient is immunocompetent but often are negative in cutaneous leishmaniasis. False-positive results may occur in patients with other infectious diseases, especially American trypanosomiasis. Treatment always is indicated for patients with mucosal or visceral leishmaniasis. Because of the high prevalence of primary antimonial resistance in India and Nepal, sodium stibogluconate should not be used for patients with visceral leishmaniasis infected in South Asia; liposomal amphotericin B or conventional amphotericin B desoxycholate should be used instead. Paromomycin intramuscular injection is approved for the treatment of visceral leishmaniasis in several countries. Treatment of cutaneous leishmaniasis should be considered, especially if skin lesions are or could become disfguring or disabling (eg, facial lesions or lesions near joints), are persistent, or are known to be or might be caused by leishmanial species that can disseminate to the naso-oropharyngeal mucosa (see Drugs for Parasitic Infections, p 848). Local wound care and treatment of bacterial superinfection also must be considered in cutaneous leishmaniasis. Miltefosine has demonstrated degrees of effcacy in visceral leishmaniasis and in New and Old World cutaneous lesions but is contraindicated in pregnancy. Meglumine antimoniate by injection is supported by the World Health Organization for treatment of leishmaniasis but is not available in the United States. Avoid outdoor activities, especially from dusk to dawn, when sand fies are most active. If possible, a bed net that has been soaked in or sprayed with permethrin should be used. The permethrin will be effective for several months if the bed net is not washed. Sand fies are smaller than mosquitoes and, therefore, can get through smaller holes. Fine-mesh netting (at least 18 holes to the inch) is needed for an effective barrier against sand fies. This particularly is important if the bed net has not been treated with permethrin. However, sleeping under such a closely woven bed net in hot weather can be uncomfortable. In the United States, the Ridley-Jopling scale is used and has 5 classifcations that correlate with histologic fndings: (1) polar tuberculoid; (2) borderline tuberculoid; (3) borderline; (4) borderline lepromatous; and (5) polar lepromatous. The cell-mediated immunity of most patients and their clinical presentation occur between the 2 extremes of tuberculoid and lepromatous forms.
Discount biltricide online mastercard. 4 2 Surveys and Questionnaires.
References
- Simmons JW, White CE, Eastridge BJ, Mace JE, Wade CE, Blackbourne LH. Impact of policy change on US Army combat transfusion practices. J Trauma. 2010;69(suppl 1):S75-S80.
- Castren-Persons M, Lipasti J, Puolakkainen P, Schroder T. Laser-induced hyperthermia: comparison of two different methods. Lasers Surg Med. 1992;12:665-668.
- Gentz J, Lindblad B, Lindstedt S, et al. Dietary treatment in tyrosinemia (tyrosinosis). With a note on the possible recognition of the carrier state. Am J Dis Child 1967;113:31.
- Ng JC, Koch MO, Daggy JK, et al: Perineural invasion in radical prostatectomy specimens: lack of prognostic significance, J Urol 172(6 Pt 1):2249n2251, 2004.