Steven N. Konstadt, MD, MBa, fa cc
- Chairman
- Department of Anesthesiology
- Maimonides Medical Center
- Brooklyn, New York
- Professor
- Anesthesiology
- Mount Sinai Medical Center
- New York, New York
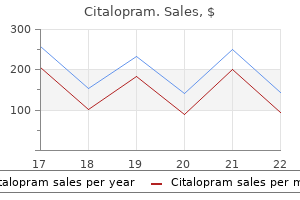
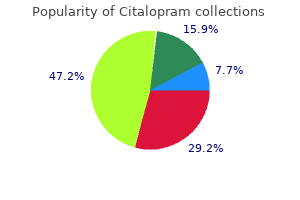
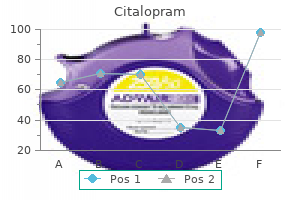
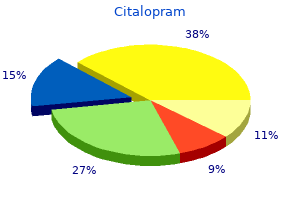
Yellowing of the sclerae treatment for scabies discount 20mg citalopram fast delivery, skin medications prescribed for migraines discount citalopram 40 mg fast delivery, and oral mucosa are all characteristic of jaundice 606 treatment syphilis purchase citalopram pills in toronto, the accumulation of bilirubin medications for ocd buy cheap citalopram online, the catabolic product of the heme moiety of hemoglobin symptoms when pregnant citalopram 20mg line. The figure illustrates general preservation of myocardial architecture with some fragmentation medications j tube generic 40 mg citalopram free shipping, more intense cytoplasmic staining corresponding to increased cellular eosinophilia, and loss of nuclei, all of which are characteristics of coagulative necrosis. The figure illustrates fatty change of the liver, which is characterized by the accumulation of intracellular parenchymal triglycerides. It is seen most frequently in the liver, heart, and kidney and is commonly secondary to alcoholism. Fatty change results from an imbalance between the uptake, utilization, and mobilization of fat from liver cells. In advanced form, primary (hereditary) hemochromatosis is characterized by the triad of cirrhosis, diabetes, and hyperpigmentation, or so-called bronze diabetes. The disease is most often caused by a mutation in the Hfe gene on chromosome 6 and is characteristically familial rather than sporadic. The skin hyperpigmentation is due largely to increases in melanin and to lesser accumulations of hemosiderin. Metastatic calcification, or deposition of calcium in previously normal tissue, is caused by hypercalcemia. In this patient, tumor metastases to the bone with increased osteolytic activity caused mobilization of calcium and phosphate, resulting in hypercalcemia. Metastatic calcification should be contrasted with dystrophic calcification, in which the serum calcium concentration is normal and previously damaged tissues are the sites of deposition. Myelin figures, cell blebs, mitochondrial swelling, and glycogen depletion are all signs of reversible injury. Nuclear changes such as pyknosis, karyorrhexis, and karyolysis are signs of cell death and are, of course, irreversible. This is limited by the extent of tissue destruction and by the regenerative capacity of the specific tissue. They are divided into three families: selectins, immunoglobulin (Ig)-family adhesion proteins, and integrins. P-selectins, stored in endothelial Weibel-Palade bodies and platelet alpha granules, relocate to the plasma membrane after stimulation by mediators such as histamine and thrombin. Intercellular adhesion molecules 1 and 2 are expressed on endothelial cells and bind to integrin molecules on leukocytes. Vascular cell adhesion molecules are similarly expressed on endothelial cells and bind to integrin molecules on leukocytes. These changes begin with a brief period of vasoconstriction, followed shortly by dilation of arterioles, capillaries, and postcapillary venules. The resultant marked increase in blood flow to the affected area is clinically manifest by redness and increased warmth of the affected area. Causes include endothelial changes that vary from contraction of endothelial cells in postcapillary venules, with widening of interendothelial gaps, to major endothelial damage involving arterioles, capillaries, and venules. Important causes of neutrophilia (increased neutrophils in the peripheral blood) include bacterial infections and other causes of acute inflammation, such as infarction. The early release of neutrophils into the peripheral blood in acute inflammation is from the bone marrow postmitotic reserve pool. There is often an increase in the proportion of less mature cells such as band neutrophils (Figure 2-1). In older individuals, chronic lymphocytic leukemia is a common cause of lymphocytosis. The most important causes of eosinophilia include allergies such as asthma, hay fever, and hives and also parasitic infections. Important causes of basophilia include chronic myelogenous leukemia and other myeloproliferative diseases. Adhesion occurs as leukocytes adhere to the endothelial surface and is mediated by the interaction of integrins on leukocytes binding to Ig-family adhesion proteins on endothelium. Chemotaxis and other forms of cellular migration are measured in an in vitro system (Boyden chamber technique) that assesses the migration of cells from an upper chamber through a microporous membrane to a lower chamber filled with a chemoattractant. This process is mediated by diffusible chemical agents (Table 2-1); movement of leukocytes occurs along a chemical gradient. Anatomic changes (1) Phagocytosis is characterized morphologically by internalization of the attached opsonized particle by pseudopodial extensions from the surface of the leukocyte, which enclose the foreign particle, forming an internalized vesicle, the phagosome. It is the coating of particulate material by substances referred to as opsonins, which immobilize the particles on the surface of the phagocyte. Intracellular microbial killing is mediated within phagocytic cells by oxygen-dependent and oxygen-independent mechanisms. Vasoactive amines (1) Histamine mediates the increase in capillary permeability associated with the contraction of endothelial cells in postcapillary venules that occurs with mild injuries. Binding of specific antigen to basophil and mast cell membrane-bound Ige (complement is not involved) 2. Binding of complement fragments C3a and C5a, anaphylatoxins, to specific cell-surface receptors on basophils and mast cells (specific antigen and IgE antibodies are not involved) 3. It is liberated from platelets, along with histamine, during the release reaction. Phospholipase A2 stimulates the release of arachidonic acid from membrane phospholipids. The complement system consists of a group of plasma proteins that participate in immune lysis of cells and play a significant role in inflammation. C5a is chemotactic, mediates the release of histamine from platelet-dense granules, induces the expression of leukocyte adhesion molecules, and activates the lipoxygenase pathway of arachidonic acid metabolism. This is a cavity filled with pus (neutrophils, monocytes, and liquefied cellular debris). This is the final result of tissue destruction, with resultant distortion of structure and, in some cases, altered function. This change is marked by the replacement of neutrophils and monocytes with lymphocytes, plasma cells, and macrophages. Because enzyme-deficient neutrophils cannot produce H2O2 and bacterial H2O2 is destroyed by bacterial catalase, H2O2 is not available as a substrate for myeloperoxidase. Chronic inflammation can occur when the inciting injury is persistent or recurrent or when the inflammatory reaction is insufficient to completely degrade the agent. It occurs in two major patterns: chronic nonspecific inflammation and granulomatous inflammation. Note the presence of lymphocytes, macrophages, and plasma cells (marked by arrows). Note the absence of caseation in this granuloma taken from a lymph node from a patient with sarcoidosis. The lesion consists of focal accumulations of altered macrophages referred to as epithelioid cells. Interaction with the antigen-specific T-cell receptor of these cells triggers the release of cytokines (especially, interferon-fi), which mediate the transformation of monocytes and macrophages to epithelioid cells and giant cells. The presence of multinucleated giant cells derived from macrophages is also characteristic. The langhans giant cell has nuclei arranged in a horseshoe-shaped pattern about the periphery of the cell and is particularly characteristic of, but not specific for, the granulomatous inflammation of tuberculosis. Giant cells, derived from macrophages, are a frequent component of granulomatous inflammation. This typical example with the nuclei arranged in the periphery in a horseshoe pattern is referred to as a Langhans giant cell. Granulomatous inflammation is the characteristic form of inflammation associated with a number of diverse etiologic agents, including: a. It requires that the surviving affected parenchymal cells have the capacity to regenerate. They include cells of the epidermis and gastrointestinal mucosa, cells lining the surface of the genitourinary tract, and hematopoietic cells of the bone marrow. Characteristically, these cells undergo few divisions but are capable of division when activated; that is, they can regenerate from G0 cells when needed. They include hepatocytes, renal tubular cells, parenchymal cells of many glands, and numerous mesenchymal cells. These cells have been considered to be incapable of division and regeneration (a view challenged by recent provocative new evidence involving stem cells). They are replaced by scar tissue (typically fibrosis; gliosis in the central nervous system) after irreversible injury and cell loss. Fibroblast growth factors promote the synthesis of extracellular matrix protein (including fibronectin) by fibroblasts, endothelial cells, monocytes, and other cells. Granulation tissue is highly vascular, newly formed connective tissue consisting of capillaries and fibroblasts; it fills defects created by liquefaction of cellular debris. As the amount of collagen in granulation tissue progressively increases, the tissue becomes gradually less vascular and less cellular. Progressive contraction of the wound also occurs, often resulting in a deformity of the original structure. Metabolic disorders, such as diabetes mellitus (associated with both susceptibility to infection and impaired circulation) 5. Dietary deficiency of ascorbic acid or protein, both of which are required for collagen formation Review Test directions: Each of the numbered items or incomplete statements in this section is followed by answers or by completions of the statement. The leukocyte count is history of progressively worsening produc14,000/mm3, with 74% segmented neutrotive cough, fever, chills, and signs of toxicity. Prominent physical findings include signs Which of the following describes the expectof consolidation and rales over the right ed findings at the affected sitefi Sputum culture is positive for (A) Fistula (abnormal duct or passage) conStreptococcus pneumoniae. An intra-alveolar necting to the abdominal wall exudate filling the alveoli of the involved (B) Granulation tissue (new vessels and portion of the lung is present. Which of the young fibroblasts) with a prominent following types of inflammatory cells is most infiltrate of eosinophils likely a prominent feature of this exudatefi A routine complete blood count perareas of abscess formation formed on a 22-year-old medical student reveals an abnormality in the differential 4. Extensive investigation results in a during the past several weeks and reports diagnosis of chronic granulomatous disease that she frequently had such episodes in the of childhood. Which of the following closely characterizes the abnormality in this cell types is most likely to be increasedfi A 16-year-old boy presents with a 24-hour formation history of severe abdominal pain, nausea, (d) Inability to kill streptococci vomiting, and low-grade fever. The accompanying figure is representative of the findings in a hilar lymph node from a 54-year-old man who sought medical care for low-grade fever, anorexia, fatigue, night sweats, weight loss, and persistent cough with bouts of hemoptysis. A chest x-ray had revealed a right apical infiltrate with beginning cavitation, and examination of the sputum had revealed acid-fast bacilli. This condition is typified by a form of inflammation that invariably includes which of the followingfi A laboratory experiment is performed to evaluate the chemotactic potential of a 8. In the laboratory, the students (c) fi2-Integrin demonstrate that the compound is a potent (d) P-selectin vasodilator and platelet antiaggregant. A 70-year-old man presents with the sud(A) Labile cells den onset of left-sided weakness, spasticity, (B) Multipotent adult progenitor cells and hyperactive and pathologic reflexes. The (c) Permanent cells most serious consequences of this disorder (d) Stable cells are the result of damage to which of the following cell typesfi In the early stages of acute inflammation, the neutrophil is the most prominent inflammatory cell. It is noteworthy that, in many instances, bacterial infections are characterized by neutrophilic infiltrates. The clinical findings are typical of acute appendicitis, another example of severe acute inflammation. Because the danger of perforation is great, early appendectomy is the treatment of choice. Suppurative or purulent inflammation is characterized by the prominent areas of edema resulting from increased vascular permeability, congestion, and a purulent (pus-containing) exudate consisting of necrotic cells and large numbers of neutrophils. In addition, other signs of acute inflammation, such as congestion, are prominent. This results in a secondary deficiency of reactive oxygen metabolites, including H2O2, which, along with halide ions, functions as a substrate for myeloperoxidase. The impaired phagocytic cell is incapable of producing H2O2, and any H2O2 produced by the microorganism itself is inactivated by endogenous catalase. In contrast, catalase-negative microorganisms, such as streptococci, are ingested and killed.
These include the following: some amount of synovial effusion associated with chronic 1 symptoms non hodgkins lymphoma citalopram 40 mg cheap. However symptoms 0f brain tumor buy cheap citalopram 40 mg line, the pattern of joint involvement may be related to the type of physical 2 medicine ball slams buy citalopram on line amex. Antigenicity of proteoglycans of human articular Degenerative changes in the interphalangeal joints lead to cartilage symptoms 7 days past ovulation buy citalopram 40mg line. Activation of cell-mediated immunity as observed by pression of cervical and lumbar nerve root with pain symptoms of strep generic citalopram 20mg without a prescription, muscle presence of numerous inflammatory cells in the synovium medicine of the prophet buy citalopram 40 mg with amex, spasms and neurologic abnormalities. Various possibilities which joints, usually with a symmetrical distribution, its systemic have been suggested are as follows: manifestations include haematologic, pulmonary, 1. The existence of an infectious agent such as mycoplasma, neurological and cardiovascular abnormalities. Eventually damage and destruction of bone and cartilage are followed by fibrosis and ankylosis producing joint deformities. The predominant pathologic lesions are found in the joints and tendons, and less often, extra-articular lesions are encountered. The proximal interphalangeal and metacarpophalangeal joints are affected most severely. Histologically, the characteristic feature is diffuse proliferative synovitis with formation of pannus. Marked thickening of the synovial membrane due to oedema, congestion and multilayering of synoviocytes. Intense inflammatory cell infiltrate in the synovial membrane with predominence of lymphocytes, plasma cells and some macrophages, at places forming lymphoid follicles. This invasion of pannus results in demineralisation and cystic resorption of underlying bone. Later, fibrous adhesions or even bony ankylosis may unite the two opposing joint surfaces. In addition, persistent inflammation causes weakening and even rupture of the tendons. Nonspecific inflammatory changes are seen in the blood vessels (acute vasculitis), lungs, pleura, pericardium, myocardium, virus, either locally in the synovial fluid or systemic infection lymph nodes, peripheral nerves and eyes. The centre of these nodules consists of an area of In response to antigenic exposure. The characteristic histologic features are villous hypertrophy of the synovium and marked mononuclear inflammatory cell infiltrate in synovial membrane with formation of lymphoid follicles at places. Infectious or suppurative arthritis is invariably an acute inflammatory involvement of the joint. Tuberculous involvement the joint space from the bloodstream but other routes of of the joints is usually monoarticular type but tends to be infection by direct contamination of an open wound or more destructive than the suppurative arthritis. Immunocompromised and commonly involved sites are the spine, hip joint and knees, debilitated patients are increasingly susceptible to and less often other joints are affected. The joint space may contain tiny grey-white loose local infection such as redness, swelling, pain and joint bodies and excessive amount of fluid. The haematogenous infectuberculous granulation tissue and cause necrosis (caries). The Gout is a disorder of purine metabolism manifested by the process begins with hyperaemia, synovial swelling and following features, occurring singly or in combination: infiltration by polymorphonuclear and mononuclear 1. There may be formation of inflammatory in which crystals of monosodium urate monohydrate may be granulation tissue and onset of fibrous adhesions between demonstrable in the leucocytes present in the synovial fluid. A family history of gout is hyperuricaemia such as in polycystic kidney disease and present in a fairly large proportion of cases indicating role of leads to urate nephropathy. The pathologic maniacute gouty arthritis, asymptomatic intervals of intercritical festations of gout include: acute gouty arthritis, chronic periods, and chronic tophaceous stage. In addition, gout tophaceous arthritis, tophi in soft tissues, and renal lesions nephropathy and urate nephrolithiasis may occur (page 692). The fundamental bioacute synovitis triggered by precipitation of sufficient chemical hallmark of gout is hyperuricaemia. A serum uric amount of needle-shaped crystals of monosodium urate acid level in excess of 7 mg/dl, which represents the upper from serum or synovial fluid. Thus, pathogenesis of gout is pathogenesis of hyperinflammation appears to include phagocytosis of crystals uricaemia. Initially, defect causing hyperuricaemia is not known, while secondary there is monoarticular involvement accompanied with denotes cases with known causes of hyperuricaemia. Acute gouty arthritis comprises about 10% cases of gout which are characterised is predominantly a disease of lower extremities, affecting by overproduction of uric acid. Other joints affected, in order rate of purine biosynthesis de novo, or an increased turnover of decreasing frequency, are: the instep, ankles, heels, of nucleic acids. Recurrent attacks of which may be either of unknown cause or are inborn errors acute gouty arthritis lead to progressive evolution into of metabolism. The deposits of urate encrust the articular increased purine biosynthesis or a deficiency of glucose-6cartilage. Tophi may be located in 855 the periarticular tissues as well as subcutaneously such as on the hands and feet. Tophi are surrounded by inflammatory reaction consisting of macrophages, lymphocytes, fibroblasts and foreign body giant cells (Fig. Three types of renal lesions are described in the kidneys: acute urate nephropathy, chronic urate nephropathy and uric acid nephrolithiasis. Pseudogout refers to an inflammatory joint involvement due to deposition of calcium pyrophosphate in the joint space. Though the two condithe condition is seen in middle-aged and elderly individuals tions have many morphologic similarities, they are best of either sex. The pathogenesis is unclear but several Giant cell tumour of tendon sheath (Nodular factors have been implicated. The of sheets of small oval to spindle-shaped cells, foamy joint effusion contains crystals of calcium pyrophosphate. Many of the spindle-shaped rhomboid crystals on the articular cartilage, ligaments, cells are haemosiderin-laden (Fig. The enlarged villi are covered by hyperplastic respectively of the same underlying process. The localised synovium and abundant subsynovial infiltrate of form of lesion is also termed xanthofibroma or benign lymphocytes, plasma cells and macrophages, many of synovioma. When the giant cells are numerous in localised which are lipid-laden and haemosiderin-laden. They were initially regarded as inflammatory in origin and hence the name synovitis. But currently cytoA ganglion is a small, round or ovoid, movable, subcutagenetic studies have shown clonal proliferation of cells neous cystic swelling. Clinically, they of wrist but may be found on the dorsal surface of foot near present with pain, swelling and limitation of movement of the ankle. It may the affected joint and may be easily mistaken for rheumatoid be the result of herniated synovium, embryologically or infective arthritis. The lesions are adequately treated by displaced synovial tissue, or posttraumatic degeneration of excision but recurrences are common. The muscle nuclei are spindle-shaped and lie at the periphery of fibre under the sarcolemma, the plasma membrane of muscle fibre. The cytoplasm of the muscle fibre contains myofilaments which are contractile elements. These together produce cross-striations in muscle fibres seen in longitudinal sections on light microscopy. Each sarcomere represents the distance between consecutive Z bands and contains the central A (anisotropic) band, and the lateral I (isotropic) bands. The major functions of striated skeletal muscle are to convert chemical energy into mechanical energy, to act as a store of energy and proteins, and to play a role in the Figure 28. The muscle, however, cannot connective tissue lined internally by flattened lining. Motor neuron cell body located in the spinal cord anterior small cyst filled with clear mucinous fluid. Bursitis occurs degeneration and regeneration; and polymyositis, dermatofollowing mechanical trauma or inflammation. Grossly, the bursal sac is neuromuscular disorders based on the part of the motor unit thick-walled and may contain watery, mucoid or granular involved is presented in Table 28. Histologically, the bursal wall is composed of dense fibrous tissue lined by inflammatory granulation tissue. The wall is infiltrated by lymphocytes, plasma cells and Site of Motor Unit Disease macrophages and may show focal calcium deposits. Unifocal Carpal-tunnel syndrome fascicles, each of which is surrounded by connective tissue 2. Grossly, the muscles but adult women are affected more often than adult men in appear normal until late in the course of disease when the ratio of 3:2. These changes amyotrophic lateral sclerosis as an example of anterior horn result in decreased neuromuscular transmission leading to cell disease, and peripheral neuropathy causing injury to 858 Figure 28. These are divided into 5 broad characteristic fasciculations of muscles of the shoulder and groups: hereditary (muscular dystrophies), inflammatory, tongue. Denervation atrophy is hereditary myopathies, also termed muscular dystrophies, pathologically characterised by groups of small angulated are briefly considered below. Myotonic Autosomal Any Slow progressive weakness Cardiac conduction Benign type dominant decade and myotonia of eyelids, defects; mental face, neck, distal limb impairment; cataracts; muscles frontal baldness; gonadal atrophy 4. FacioscapuloAutosomal 2nd-4th Slowly progressive weakness Hypertension Benign humeral type dominant decade of facial, scapular and humeral muscles 5. Limb-girdle Autosomal Early childSlowly progressive weakness Cardiomyopathy Variable type recessive hood to of shoulder and hip progression adult girdle muscles 6. Common to all forms of differences in inheritance pattern, age at onset, clinical muscular dystrophies are muscle fibre necrosis, features, other organ system involvements and clinical regenerative activity, replacement by interstitial fibrosis course. Frequently there is history of antecedent trauma which may reticuloendothelial system, the glia and the supporting bring the tumour to attention of the patient. Molecular and cytogenetic studies in many soft tissue included for the purpose of categorisation of their tumours tumours reveal chromosomal abnormalities and mutations in are: fibrous tissue, adipose tissue, muscle tissue, synovial genes which can be used as a marker for diagnosis and tissue, blood vessels and neuroectodermal tissues of the histogenesis. Most of the soft tissue tumours occur sporadically; however these tissues are embryologically derived from mesoderm, there are a few examples which are components of genetic except those of peripheral nerve which are derived from ectosyndromes. Tumours of smooth muscle tissue, blood vessels and syndrome, Osler-Weber-Rendu syndrome etc. Benign soft tissue tumours are about 100 times more Benign: these soft tissue tumours generally do not recur and common than sarcomas. Instead, Intermediate, locally aggressive: these tumours are locally sarcomas originate from the primitive mesenchymal cells destructive, infiltrative and often recur but do not having the capacity to differentiate along different cell pathmetastasise. As discussed in Chapter 8, soft tissue sarcomas excision; for example desmoid tumour. Common example in tiation and grading of soft tissue sarcomas are important this category is dermtofibrosarcoma protuberans. The metastatic rate in low-grade general features: sarcomas is about 2-10% and in high-grade sarcomas is Superficially-located tumours tend to be benign while 20-100%. Cell patterns: Several morphological patterns in which while benign tumours are selectively avascular. Approximately 15% of soft tissue tumours occur in iii) Herringbone pattern: is seen in fibrosarcoma in which children and include some specific examples of soft tissue the tumour cells are arranged like the vertebral column of sarcomas. Cell types: After looking at the pattern of cells described determining histogenesis, or for diagnosis and prognosis. Different staging systems for soft tissue sarcomas (cigar-shaped) nuclei and more intense eosinophilic have been described but two of the most accepted staging cytoplasm. Based on differential diagnosis made on routine Fibromas, fibromatosis and fibrosarcoma are benign, tumourmorphology, the panel of antibody stains is chosen for like, and malignant neoplasms respectively, of fibrous applying on paraffin sections for staining. A keloid is a progressive fibrous overgrowth in response to cutaneous injury such as burns, incisions, insect bites, vaccinations and others. Grossly, the keloid is a firm, smooth, pink, raised patch from which extend claw-like processes (keloid-claw).
The instructors will assist you in developing skills to differentiate the rhythms required for successful completion symptoms zoloft dosage too high buy citalopram 20mg without prescription. Ventricular Fibrillation $ Chaotic treatment brown recluse spider bite purchase citalopram with amex, disorganized electrical depolarization of the ventricles 4 medicine in balance buy cheap citalopram online. Atrial Flutter $ No definable P waves; "sawtooth" appearing flutter waves from atrial depolarization treatment statistics generic 40mg citalopram with amex. This example is regular due to it dropping every other beat (2:1 conduction nd ratio) medicine used to stop contractions citalopram 40 mg free shipping. This example is irregular due to it dropping every so often (variable conduction ratio) treatment 2 degree burns order discount citalopram online. The emphasis in equine cardiology is mostly on diagnosis and prognosis, rather than the treatment of cardiac disease. This lecture aims to help you interpret your clinical examination in order to provide likely differentials, and to understand the significance of those differentials and when further investigation is warranted. History & Signalment the most common reason for presentation of a horse for a cardiovascular workup is poor performance/recovery. Despite this, lameness and respiratory disease/ dysfunction are far more common causes of poor performance than cardiovascular disorders. Cardiovascular abnormalities are often detected on routine clinical or prepurchase examination, leading to a full cardiovascular workup. A massive functional cardiac reserve means that horses rarely present with signs of obvious cardiac failure. Clinical Examination Remember to include a thorough examination of all body systems. In a horse presented for poor performance, lameness and respiratory evaluations are always warranted. Oedema can occur in the brisket region/under the cranial abdomen and in the prepuce of horses with cardiac failure. Distal limb oedema can occur with cardiac disease, although other causes (hypoproteinaemia, vasculitis etc) are far more common. Palpation of the facial artery (under the jaw) is the usual site for assessment, though the transverse facial artery (located just ventral and caudal to the lateral canthus of the eye) is also a useful site. Pulse strength represents the difference between systolic and diastolic pressures. Low output cardiac failure may result in pale mucous membranes and a prolonged capillary refill time. Cyanosis may be apparent with right to left shunting such that occurs in some congenital disorders. These causes need to be distinguished from pulses that are referred from the carotid arteries. Always listen to the left and right sides, and always include the lung fields in your examination. The diaphragm is best for picking up high frequency sounds, the bell for lower frequency sounds. Normal resting heart rate varies from 25-45 beats per minute in adults and 60-80 bpm in foals. S1 (Lub) is associated with closure of the atrioventricular valves (the left = mitral, the right = tricuspid) and marks the beginning of systole (ventricles contracting). S2 is associated with closure of the semilunar valves (aortic and pulmonary), as blood slows in the aorta and pulmonary artery, and marks the end of systole. Systole Diastole Systole In addition to the two main heart sounds, two other normal sounds, S3 and S4, can be heard in some horses (usually fit horses). Sounds associated with each of the valves can be heard in different regions on the chest wall. These regions do not necessarily correlate with the position of the underlying valve. This area is the best place to listen for S3, and sounds associated with the mitral valve. Move cranially under the triceps muscle to around the 4PthP intercostal space, midway between the point of the shoulder and olecranon. This is the best place to listen for sounds associated with the tricuspid valve, and S1 will be loudest in this area. The normal transient heart sounds (S1-S4) vary in intensity depending on fitness, body condition, and individual variation. Consolidated lung between the heart and thoracic wall may result in louder sounds that are heard over a wider area than normal. Intrathoracic masses may change the position of the heart within the thoracic cavity and change the loudness or positioning of heart sounds at the chest wall. They are caused by turbulent blood flow which results in vibration of cardiac structures. The position is correlated with a valvular region (see above) or can be expressed as being toward the base or apex region of the underlying heart. Precordial thrills are associated with high velocity turbulence & significant disturbance of flow. Functional murmurs High velocity blood flow and large vessel diameter increase the potential for turbulent flow. The properties of the equine heart (large chambers & vessels, large stroke volume) mean that turbulent flow can readily occur even when pathology is not present. Non-pathological murmurs associated with normal blood flow are relatively common especially in fit, young horses. They are usually heard best over the base of the heart on the left side of the chest (pulmonary and aortic areas) and are localized (do not radiate). These murmurs are very short in duration and high pitched, can often be heard over both sides of the chest, and occur between S2 and S3. Additional Diagnostic Procedures 1) Laboratory medicine: A complete blood profile is useful in all cases of suspected cardiac disease to determine the presence of inflammation, infection and/or systemic disease. Changes in white cell count and differential may support a diagnosis of bacterial endocarditis or pericarditis. A lymphocytosis +/monocytosis may support a diagnosis of viral pericarditis or myocarditis. High plasma fibrinogen indicates an inflammatory process is present, though this is not specific to the heart. The levels of these enzymes may be increased when active myocardial damage is present, although specificity and sensitivity of these tests is questionable. Plasma cardiac tropinin I (cTnI) is a sensitive and (fairly) specific indicator of myocardial damage and/or inflammation in horses. There is a widespread Purkinje network within the ventricles of the horse resulting in multiple depolarisation points across the myocardium. Alternatively, in the Y lead system the positive electrode is attached over the xiphoid and the negative over the manubrium. A neutral electrode is required in mains powered machines, attached at any convenient site. The P wave may change morphology from beat to beat in normal horses (wandering pacemaker). The T wave varies greatly in polarity and morphology in normal horses but should be the same or similar in an individual horse. The heart score has been used as an indicator of ventricular size, and a predictor of performance. It is often associatedst with high vagal tone, and is sometimes seen in fit athletic horses at rest. It is rarely if ever pathological, and is abolished at higher heart rates in normal horses. It occurs commonly in normal horses at rest (up to 44% of normal horses), and is a homeostatic mechanism to reduce cardiac output at rest. Pathological arrhythmias such as atrial fibrillation sound irregularly irregular, and will not be abolished at higher heart rates. Treatment can be attempted with vagolytic drugs (often unsuccessful), corticosteroids are indicated (dexamethasone 0. It is usually associated with changes in vagal tone in horses at rest, or in the period just following exercise. This arrhythmia is usually abolished at higher heart rates, though in some cases it may be associated with poor performance. In severe cases an escape beat or rhythm originating in the junctional or ventricular tissue may be generated. Treatment involves correcting the underlying cause, corticosteroids, sympathomimetic drugs, or even pacemaker implantation in persistent cases. If they are more frequent at rest, associated with runs of paroxysmal supraventricular tachycardia, or the horse presents for poor performance, further investigation is warranted. Corticosteroid therapy (~4 weeks of dexamethasone or prednisolone) may be useful in refractory cases, or when myocardial inflammation is suspected. It occurs most commonly in athletic horses without underlying cardiac disease, but also occurs in horses with cardiac disease, particularly where atrial enlargement has occurred. Large atria and high vagal tone allow the rhythm to perpetuate in horses without underlying cardiac disease. However, atrial contraction can contribute up to 25% of ventricular filling at maximal exercise. The most common presentation however is that of sudden loss of performance in a standardbred or thoroughbred racehorse. Atrial fibrillation can be paroxysmal (reverts spontaneously within 24-48h) or sustained. The ventricular response rate varies, but is usually similar to normal sinus rate in horses without underlying cardiac disease. An echocardiogram is indicated to rule out the presence of primary cardiac disease, in particular atrial enlargement. Cardioversion is generally recommended for horses performing high intensity athletic activities, or if the average maximal heart rate during exercise (at a level mirroring the horses intended use) is greater than 220/ minute. The antiarrhythmic drug quinidine is most commonly used for conversion to sinus rhythm. Quinidine sulfate is administered at 22mg/kg via nasogastric tube every 2 hours until a maximum dose of 40-60g (4-6 treatments for a 500kg horse) is reached, toxic or adverse reactions occur, or conversion is achieved. Alternatively, dosing may be continued with the frequency reduced to every 6 hours until conversion is affected. Digoxin may be added to the regimen in refractory cases or in horses that are tachycardic/have previously become severely tachycardic during a conversion attempt. Side effects of quinidine therapy commonly encountered include: Depression sweating, paraphimosis flatulence colic, diarrhea tachycardia Reduced myocardial contractility and congestive heart failure can occur in horses with underlying myocardial dysfunction. Prognosis is good in horses with minimal underlying heart disease 90% of these horses are converted to normal sinus (quinidine or electrical cardioversion). If this happens, it usually does so within the first 24 48 hours (paroxysmal atrial fibrillation). Horses that do not convert to sinus rhythm can function normally as breeding animals, and can usually tolerate mild athletic activity (dressage, pony club etc. A complete cardiovascular examination is indicated, including electrocardiography (24 hour holter, exercise test) an echocardiogram and cardiac isoenzymes (cTnI). If R on T phenomenon is present, antiarrhythmic drug therapy is indicated as this may predispose the horse to ventricular tachycardia or ventricular fibrillation. Clinical examination will often reveal signs of severe systemic disease (colic, toxaemia etc. Clinical signs of congestive heart failure may develop due to the high heart rate. This is considered an extremely unstable rhythm, with progression to ventricular fibrillation possible. Antiarrhythmic therapy for ventricular tachycardia is indicated if the rate is excessively high, the rhythm is multiform, or R on T complexes are detected.
Theoretically medicine wheel native american purchase 40 mg citalopram otc, a person who carries a robertsonian translocation with chromosome 21 and a second acrocentric chromosome has a 1 in 3 chance of having a child with trisomy 21; however medications for ptsd buy generic citalopram 20 mg on-line, the risk of a live birth of a child with Down syndrome is actually much less chi infra treatment generic citalopram 20 mg amex, presumably because of a high incidence of spontaneous abortion of such fetuses medicine you can give cats effective citalopram 40 mg. The important point is that a robertsonian translocation predisposes to a hereditable form of Down syndrome symptoms anxiety order citalopram cheap. Affected patients often have multiple pulmonary infections and pancreatic insufficiency with steatorrhea and failure to thrive treatment bulging disc buy citalopram pills in toronto. Increased concentration of chloride in sweat and tears is characteristic, and the sweat test is an important diagnostic adjunct. Abnormalities of mitochondrial inheritance typically involve genes that code for enzymes of oxidative phosphorylation. Multifactorial disorders are among the most common familial abnormalities and are much more common than monogenic disorders. In addition, there is common occurrence of congenital heart disease, especially defects of the endocardial cushion (atrioventricular valve malformations and atrial and ventricular septal defects), and increased susceptibility to infection. Many patients with Down syndrome who are older than 35 years of age show clinical signs, symptoms, and pathologic findings of Alzheimer-type dementia, with an incidence much higher than in the general population. The clinical findings are those of type I Gaucher disease, which is a manifestation of glucocerebrosidase deficiency. The disorder is most often seen in persons of European (Ashkenazic) Jewish lineage. Prominent findings include bone pain and fractures, easy bruising, hepatosplenomegaly, anemia, and thrombocytopenia. The disease is highly variable in its clinical manifestations, and assays of chitotriosidase and angiotensin-converting enzyme, markers of macrophage proliferation, are useful measures of the extent of disease and of its control. The patient has homogentisic oxidase deficiency, a rare inborn error of metabolism (actually the first such disorder described by Garrod in 1902), clinically manifest by alkaptonuria and ochronosis. The term ochronosis refers to pigment deposition in multiple tissues, most prominently in cartilage and connective tissue. The concentration of phenylalanine in affected infants is usually normal at birth and increases rapidly during the first days of life. False-negative results are common immediately after birth but are rare on the second and third days of life. The phenomenon of earlier and more severe manifestations of a disorder in successive generations (anticipation) is a characteristic of many trinucleotide repeat disorders, the best known examples of which are fragile X syndrome (discussed in this chapter) and Huntington disease (described in this clinical scenario and further discussed in Chapter 23). The degree of expansion is closely related to the gender of the parent with the genetic abnormality. They are identified by cell-surface glycoproteins specific for both cell type and stage of differentiation. They populate the paracortical and deep medullary areas of lymph nodes and periarteriolar sheaths of the spleen. Neither specific sensitization nor antibody is involved in this type of cell killing. These derivatives of peripheral blood monocytes are members of the mononuclear phagocyte system of cells. Macrophages secrete a variety of cytokines, including interleukin-1 (Il-1), as well as other products, such as acid hydrolases, neutral proteases, and prostaglandins. Dendritic cells of lymphoid tissue are characterized by dendritic cytoplasmic processes. In contrast to macrophages, dendritic cells are poorly phagocytic; however, like macrophages, dendritic cells are antigen-presenting cells. Ultrastructural characteristics include the presence of Birbeck granules, tennis racketshaped cytoplasmic structures. The final lytic form of activated complement is the result of a series of enzymatic cleavages and recombinations of cleavage products. Adaptive immune responses are mediated by B and T lymphocytes and are related to well-known reactions with specific antigens. The classification of Gell and Coombs divides hypersensitivity reactions into four types (Table 5-2). Immunoglobulin e (Ige) antibody production by IgE B cells is stimulated by antigen. On subsequent exposure, antigen (allergen) reacts with bound IgE antibody (complement is not involved), resulting in cytolysis and degranulation of basophils or tissue mast cells. This reaction requires bridging (cross-linking) of adjacent IgE molecules on the mast cell surface. Degranulation results in histamine release, which increases vascular permeability. Various other substances are produced, many of which are vasoactive or smooth muscle spasm-inducing. Chemotactic substances recruit eosinophils, resulting in tissue and peripheral blood eosinophilia. Allergic or atopic reactions, such as seasonal rhinitis (hay fever), allergic asthma, or urticaria (hives). Rapid onset of urticaria, bronchospasm, laryngeal edema, and shock after exposure to an offending antigen is characteristic. Angioedema, which is acute edema of cutaneous or mucosal structures, most commonly involving the lips and eyelids. Hereditary angioedema is caused by deficiency of C1 esterase inhibiter and is not a manifestation of type I hypersensitivity. Complement-fixing antibodies react directly with antigens that are integral components of the target cell. The interaction of complement with the cell surface results in cell lysis and destruction. The antigens involved are usually localized to tissue basement membranes or blood cell membranes. Clinical examples include warm antibody autoimmune hemolytic anemia, hemolytic transfusion reactions, and hemolytic disease of the newborn (erythroblastosis fetalis), in which the antigens are components of red blood cell membranes, and Goodpasture syndrome (antiglomerular basement membrane antibody disease), in which the pulmonary alveolar and glomerular basement membranes are affected. The free Fc portion of the antibody molecule reacts with the Fc receptor of a variety of cytotoxic leukocytes, most importantly nK cells. Exogenous antibody produced in response to exposure to antigen combines with antigen, resulting in circulating antigen-antibody complexes. Immune complexes are most often removed by cells of the mononuclear phagocyte system without adverse effect. In other cases, insoluble aggregates of immune complex are deposited in vessel walls or on serosal surfaces or other extravascular sites. This involves smaller immune complexes that are less easily removed by the mononuclear phagocyte system. In the past, antibody-containing foreign serum (most often horse serum) was administered therapeutically for passive immunization against microorganisms or their toxic products. Because of the danger of serum sickness, this mode of therapy is no longer employed. Arthus reaction is a localized immune complex reaction that occurs when exogenous antigen is introduced, either by injection or by organ transplant, in the presence of an excess of preformed antibodies. Immune complex-mediated glomerular diseases include poststreptococcal glomerulonephritis, membranous glomerulonephritis, and lupus nephropathy. Three basic patterns of graft rejection are well illustrated by rejection following kidney transplantation. Rejection is primarily antibody-mediated and occurs in the presence of preexisting antibody to donor antigens. Rejection is a localized Arthus reaction marked by acute inflammation, fibrinoid necrosis of small vessels, and extensive thrombosis. Rejection may occur months to years after an otherwise successful transplantation. Rejection is characterized histologically by marked vascular fibrointimal proliferation, often resulting in a small, scarred kidney. It is becoming more common with the success of immunosuppression in overcoming acute rejection. This is a significant problem in bone marrow transplantation because immunocompetent cells are transplanted in this procedure. This disorder occurs in male infants but usually does not manifest clinically until after 6 months of age because of the persistence of maternal antibodies. Failure of antibody synthesis caused by a block in maturation of pre-B cells to B cells due to a mutation in the B cell tyrosine kinase (Btk) gene. A propensity for recurrent bacterial infections with organisms, such as pneumococci, streptococci, staphylococci, and Haemophilus influenzae. Resistance to viral and fungal infections or phagocytosis and killing of bacteria by neutrophils is not affected. The most common inherited B cell defect, isolated IgA deficiency, occurs in approximately 1 in 700 persons. It may also be associated with infections, especially those involving mucosal surfaces, and manifest as recurrent upper respiratory tract infections and frequent episodes of diarrhea. This diverse group of disorders is caused by failure of terminal B-cell maturation, resulting in diminution in the number of plasma cells and thus hypogammaglobulinemia. This congenital t-cell deficiency results from aberrant embryonic development of the third and fourth branchial arches, leading to hypoplasia of the thymus and parathyroid glands, as well as abnormalities of the mandible, ear, and aortic arch. Clinical manifestations include recurrent viral and fungal infections and tetany from hypoparathyroidism with hypocalcemia. Marked deficiency of both B and t cells manifests as profound lymphopenia and severe defects in both humoral and cell-mediated immunity. Characteristics include eczema, thrombocytopenia, recurrent infections, and poor antibody response to polysaccharide antigens. It is characterized by normal or elevated levels of IgM, but failure of isotype switching to IgG, IgA, or IgE. Chapter 5 Immune Dysfunction 75 (2) Low-level virion production, with resultant infectivity, occurs even during the latent period. Severe immunodeficiency manifested by opportunistic infection with organisms such as Pneumocystis jiroveci (Pneumocystis carinii), Cytomegalovirus, Mucor species, and typical and atypical mycobacteria such as Mycobacterium avium-intracellulare; other opportunistic infections often found include Candida, Cryptosporidium, Coccidioides, Cryptococcus, Toxoplasma, Histoplasma, and Giardia infections (Figure 5-1). The foamy exudate filling the alveoli contains the causative organisms, which can be demonstrated by silver staining. Note the characteristic atypical spindle cells and red cell containing slit-like vascular spaces (arrows). Antibodies to the proteins coded by the genes of retroviral gag, env, and pol regions can be demonstrated, especially antibodies to the gp120 and p24 proteins. Examples include a number of autoimmune disorders, including autoimmune hemolytic anemia, hashimoto thyroiditis, idiopathic adrenal atrophy, and a group of disorders referred to as connective tissue diseases. Host antigens may be recognized as nonself if modified by infection, inflammation, or complexing with a drug. Antigens usually isolated from the immune system may be exposed by trauma or inflammation and become recognized as foreign. Many autoimmune disorders are characterized by the presence of specific autoantibodies, antibodies directed against host tissue. The demonstration of autoantibodies is presumptive (but not entirely conclusive) evidence of the autoimmune nature of a disorder. Some hlA antigens are associated with increased incidence of certain autoimmune disorders. Some viruses apparently trigger autoimmune islet cell inflammation and resultant type 1 diabetes. They may be of autoimmune origin; antinuclear antibodies (AnAs) and various other autoantibodies are often present. Skin rashes, including a characteristic butterfly rash over the base of the nose and malar eminences, often with associated photosensitivity d. Raynaud phenomenon, manifested by vasospasm of small vessels, most often of the fingers. Diffuse interstitial pulmonary fibrosis, manifested as interstitial pneumonitis or diffuse fibrosing alveolitis g. In the spleen, perivascular fibrosis with concentric rings of collagen around splenic arterioles results in a characteristic onion-skin appearance. Glomerular changes varying from minimal involvement to severe diffuse proliferative disease with marked subendothelial and mesangial immune complex deposition, endothelial proliferation, and thickening of basement membranes; can be indistinguishable from idiopathic membranous glomerulonephritis. Biologic false-positive tests for syphilis (due to anticardiolipins, a form of antiphospholipid antibody) occur in approximately 15% of patients. The initial presentation usually includes skin changes, polyarthralgias, and esophageal symptoms. Visceral organ involvement, especially of the esophagus, gastrointestinal tract, kidneys, lungs, and heart (1) the esophagus is frequently affected, and dysphagia is common. Involvement of salivary glands, often with bilaterally enlarged parotids diffusely infiltrated by lymphocytes and plasma cells. This cellular infiltration can partly or completely obscure the parenchyma of the parotid gland and can mimic, or in some cases lead to , malignant lymphoma.
Buy generic citalopram 40 mg on-line. How to deal with Depression and Anxiety? By Dr Ashish Mittal I Hindi.
References
- Perkins CJ, Kahya E, Roque CT, et al. Fluid-attenuated inversion recovery and diffusion- and perfusion-weighted MRI abnormalities in 117 consecutive patients with stroke symptoms. Stroke 2001;32:2774-81.
- Losa M, Valle M, Mortini P, et al. Gamma knife surgery for treatment of residual nonfunctioning pituitary adenomas after surgical debulking. J Neurosurg 2004;100(3):438-444.
- Duncan WJ: Left ventricular rhabdomyoma. Pediatr Cardiol 1983; 4:170-171.
- Schwamm LH, Pancioli A, Acker JE 3rd, et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Stroke 2005;36: 690-703.
- Wei S, Asamura H, Kawachi R, Sakurai H, Watanabe S. Which is the better prognostic factor for resected non-small cell lung cancer: the number of metastatic lymph nodes or the currently used nodal stage classification? J Thorac Oncol 2011;6(2):310-8.