Professor Julian Bion
- Professor of Intensive Care Medicine
- University Department of
- Anaesthesia & Intensive Care Medicine,
- N5 Queen Elizabeth Hospital,
- Edgbaston,
- Birmingham
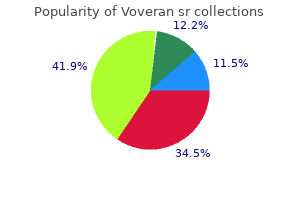
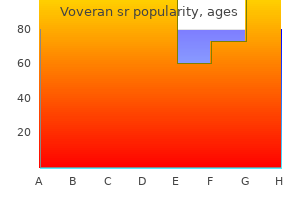
Iron in haem has six coordinating valencies: four link the iron to nitrogen atoms in each pyrrole ring back spasms 33 weeks pregnant voveran sr 100 mg without a prescription, whereas the remaining two link haem to histidine residues in the globin chain muscle relaxant withdrawal generic 100mg voveran sr amex, the distal bond being unstable and easily replaced by oxygen to form oxyhemoglobin muscle relaxant apo 10 purchase 100 mg voveran sr fast delivery. The mitochondria are also the site ofthe citric acid cycle spasms of the heart buy generic voveran sr 100mg on line, which supplies succinate muscle relaxant no drowsiness voveran sr 100 mg. The 2 mature red cell muscle relaxant for headache generic 100 mg voveran sr with amex, which lacks mitochondria, is therefore unable to synthesize haem. A number of porphyrins are formed by side reactions during the synthesis of protoporphyrin. In the porphyrias, many of these compounds accumulate in the major sites of sites of haem synthesis the liver and the red cells 1. Moreover, the entry of iron into the cell and its incorporation into haem are regulated so that the normal cell obtains sufficient iron for its needs, but not more. Its activity reaches a peak in the polychromatic normoblast and then diminishes so that no activity is present in the mature cell. Increased amounts of the intermediates of haem synthesis accumulate, the disorders being classified by whether the effects are predominantly in the liver or the erythron. Large amounts of porphyrinogens accumulate,and their conversion by spontaneous oxidation to photoactiveporphyrins leads to severe, and disfiguring, cutaneous photosensitivity and dermatitis, as well as a hemolytic anaemia with splenomegaly. Increased amounts of uroporphyrin and coproporphyrin,mainly type I, are found in bone marrow, red cells,plasma, urine and faeces. Ring sideroblasts have been found in the marrow in some cases but rarely in large numbers. The age of onset and clinical severity of the disease are highly variable,ranging from non immune 3 hydrops fetalis to a later onset in which there are only cutaneous lesions. Treatment, includingavoidance of sunlightand splenectomy to improve red cell survival,is only partially effective. High level blood transfusions tosuppress erythropoiesis (combined with iron chelation therapy)have been used to reduce porphyrin production sufficiently toabolish the clinical symptoms. Molecular analysis of the ferrochelatase gene has revealed a variety of missense, nonsense and slicing mutations as well as deletions and insertions. Expression of the gene is variable, and photosensitivity and dermatitis range from mild or absent to moderate in degree. There is little hemolysis, buta mild hypochromic anaemia may occur, and accumulation of protoporphyrins can occasionally lead to severe liver disease. In the urine, uroporphyrin and heptacarboxyl porphyrin predominate with lesser amounts of coproporphyrin andpenta and hexacarboxyl porphyrin. It is precipitated in middle or later life, more often in men than women, by factors such as liver disease, alcohol excess or oestrogen therapy. Removal of the ironby repeated phlebotomy is standard treatment usually leading to remission 1. While in the nucleus, it undergoes a number of modification s first, the introns are removed and the exons are spliced together this too is a complex, multistep process involving several different proteins that constitute the spliceosome. When the ribosomes reach the termination codon translation ceases, thecompleted globin chain is released, and the ribosomal subunitsfall apart and are recycled. Individual globin chains combinewith haem, which is synthesized through a separate pathway,and with themselves to form definitive haemoglobinmolecule. The hemoglobin molecule loads oxygen on a one to one basis, one molecule of hemoglobin to one molecule of oxygen in the oxygen rich environment of the alveoli of the lungs. Hemoglobin becomes saturated with oxygen, oxy hemoglobin, and has a high affinity for oxygen in this pulmonary environment, because the network of capillaries in the lungs makes the diffusion of oxygen a rapid process. As the molecule transits through the circulation, deoxy hemoglobinis able to transport oxygen and unload to the tissues in areas of low oxygen affinity. As hemoglobin goes through the loading and unloading process, changes appear in the molecule. Oxygen dissociation curve has a sigmoid shape under normal condition only upper part is used. Under influence of acidosis curve is shifted to the right and more oxygen is released. In anemic patients, stroke volume of heart is in increased heart beats faster in addition 2,3diphosphoglycerate concentration increase to facilitate the oxygen dissociation in tissues. Present in very small amount at birth and reach the adult level (1,5 3,5) during first year. This conversion is the basis for most of the colorimetric procedures used to measure hemoglobin,and it depends on a versatile and viable hemoglobin compound. Hemoglobin that are physiologically abnormal have a higher oxygen affinity and produce conditions that are usually toxic to the human body. These abnormal hemoglobins include; methemoglobin,sulfhemoglobin, and carboxy hemoglobin. The amounts of any of these abnormal hemoglobins in the bloodstream can be potentially fatal. Often, the production of abnormal hemoglobins results from accidental or purposeful ingestion or absorption of substances, drugs, and so on that are harmful. In the 3+ abnormal hemoglobin methemoglobin, iron has been oxidized to the Fe state, 10 which is no longer capable of binding oxygen. Methemoglobin builds up in the circulation and if the level is above 10%, individuals appear cyanotic, having a blue color, especially in the lips and fingers. Aniline drugs and some antimalarial treatments may induce a methemoglobinemia in individuals who are unable to reduce methemoglobin. Hemoglobin M, an inherited condition arising from an amino acid substitution, may also result in cyanotic conditions. As a hemoglobin derivative, carboxyhemoglobin has an affinity for carbon monoxide that is 200 times greater than for oxygen; therefore, no oxygen is delivered to the tissues. For this reason, carbon monoxide poisoning, either deliberate or accidental, is efficient and relatively painless. Sulfhemoglobin can be formedon exposure to agents such as sulfonamides or sulfa containing drugs. The affinity of sulfhemoglobin for oxygen is 100 times lower than that of normal hemoglobin. Unstable hemoglobin is rare and cause chronic hemolytic anemia of varying severity with intravascular hemolysis. The thalassaemias are classified as or,depending on which pair of globin chains is synthesized (8). The sickle beta globin result from substituation of valine for glutamic acid at position 6 in? However, in a health survey of apparently normal men and women in Britain, mean Hb values of 145 g/l for men and 128 g/l for women have been reportedthe lower normal limits for Hb. It is possible that some have nutritional deficiencies, especially iron deficiency, without clinical effects. Apart from a hormonal influenceon hemopoiesis, iron deficiency is likely to be a factor influencing the difference; the extent to which menstrual blood loss is a significant factor is not clear because a loss of up to 100 ml of blood with eachperiod may lead to iron depletion without causing anaemia. Serum ferritin decreases in early pregnancy and usually remains low throughout out pregnancy even with supplementary iron is given. In the elderly, the difference in Hb between men and women is less than in younger subjects, so that a difference of 20 g/l in younger age groups isreduced to 10 g/l or less in the elderly. There is a concomitant increase in serum iron in women, although serum ferritin levels remain higher in men thanIn women. Factors which contribute to the lower Hb I the elderly include renal insufficiency, inflammation, testosterone deficiency, diminished erythropoiesis, stem cell proliferative decline and 13 myelodysplasia. Moderate or severe anemia should never be attributed to ageingnper se until underlying disease has been excluded; however, a significant number of elderly subjects with anemia have no identifiable clinical or nutritional causes. The difference in position of the arm during venous sampling, whether dependent or held at atrial level, can also affect theHct. These aspects highlight the relevance of using a standardized method for blood collection, although this is not necessarilyPracticable in routine practice. Studies of diurnal variation of serum erythropoietin have shown conflicting results. Pronounced, but variable, diurnal variations are seen in serum iron and ferritin and in patients taking iron containing supplements. Severalhaematologicalparameters can affect or be influenced by physical activity including blood cells and coagulation mechanisms. For example endurance athletes may develop so called sports anemia?, which is thought to be the result of increased plasma volume. Increasing oxygen deliveryby raising thehaematocrit is a simple acute method to improve athletic performance. Legal means of raising the haematocrit include altitude training and hypoxic tents. Endurance athletes may also have decreased levels of serum iron and ferritin, possibly associated with loss of iron in sweat. Some effects may be transient and their severity varies between individuals as well as by the number of cigarettes smoked. This is probably at least in part a consequence of the accumulation of carboxy hemoglobin in the blood together with a decrease in plasma volume. After a single cigarette, the carboxyhemoglobin level increases by about 1%,and in heavy smokers the carboxy hemoglobin may constitute 4?5% of the total Hb. The leucocyte count increases, largely as a result of an increase in the neutrophils and neutrophil function maybe affected. Studies of platelet aggregation and adhesiveness have given equivocal results, but there appears to be a consistent increase in platelet turnover with decreased platelet survival and increased plasma b thromboglobulin. Elevated fibrinogen concentration (with increased plasma viscosity) and reduced proteins have been reported, but smoking does not seem to have any consistent effects on. However used in under resourced laboratories may be limited by the need for a specialized centrifuge and a reliable supply of capillary tubes. Accuracy of Microhaematocrit the microhematocrit method has an adequate level of accuracy and precision for clinical utility. However, attention must be paid to a number of factors that may produce an inaccurate result. To ensure adequate oxygenation and sample mixing, the free air space above the sample should be more than 2o % of the container volum. Capillary Tubes Variation of the bore of the tubes may causeserious errors if they are not within the narrow limits of defined specifications that should be met by manufacturers: length 75 0. Efficiency of packing should also be tested by centrifuging samples of normal and polycythaemic blood for varying times from 5 to 10 min to determine the minimum time for complete packing ofThe red cells. To avoid errors in reading with the special reading device, a magnifying glass should be used. White cells and platelets (the buffy coat) must be excluded as far as possible from the reading of the packed red cell volume. If a special reading device is not available, the ratio of red cell column to whole column can be calculated from measurements obtained by placing the tube against arithmetic graph paper or against a ruler. Plasma trapping is increased in macrocytic anemias,spherocytosis, thalassemia, hypochromic anemias and sickle cell anemia;it may be as high as 20% in sickle cell anemia if all the cells are sickles Basic hematological techniquesInternationalCouncil for Standardization in. This research is aimed to study mean hemoglobin and packed cell volume among student of Sudan University of science and technology to see if there is a differences in the results of these two essential laboratory tests between males and female, in other hand, to compare with international reference values for the same age group. Sealing the tube by heating is not recommended because the seals tend to be tapered and there is the likelihood of lysis. After centrifugation for 5 min, measure the proportion of cells to the whole column. Five hundred student were participated in this study,(251) were males (51%) and (249) were females (49%). The result of this study show that mean of hemoglobin concentrations in males was 12. Other study done in south Africa show that the normal value of hemoglobin was (11. There is a difference between above study due to difference in climate, nutritional and ethnic factors. Our research done from adult healthy population hence be suggest other may fellows to study from children. Frank Firkin, Colin Chesterman, David Penington and Bryan Rushde, th Gruchy s Clinical Haematology in Medical Practie,5 edition. Microfilariae can be evaluated for morphometric features with high magnification (40 100x obj). You?ll also learn about neutropenia, anemia, and thrombocytopenia 3 kinds of blood deficiencies. These cells also have a protein in them called hemoglobin, which is what makes red blood cells red. For example, you might not have enough white blood cells, or your platelet count could be lower than normal. To prevent infections, you need to keep germs (like bacteria and viruses) out of your body. So when your platelet count is low, talk with your doctor or nurse before you take any new medicines. Check the list at the end of this fact sheet for names of common medicines that have aspirin in them. Brancati Initially submitted November 14, 2007; accepted for publication July 14, 2008. Several lines of evidence support the notion that elevated blood viscosity may predispose to insulin resistance and type 2 diabetes mellitus by limiting delivery of glucose, insulin, and oxygen to metabolically active tissues. Whole blood viscosity was estimated by using a validated formula based on hematocrit and total plasma proteins at baseline.
In situations where faecal contamination of the domestic environment is high spasms quadriceps discount 100 mg voveran sr otc, the majority of cases of endemic disease probably occurs either by human to human transmission infantile spasms 2013 buy voveran sr in united states online, or from the human to human transmission of pathogenic agents which have multiplied in the environment kidney spasms no pain discount voveran sr master card. Acute watery diarrhea: this term refers to diarrhea characterized by abrupt onset of frequent muscle relaxant 503 purchase line voveran sr, watery muscle relaxant for headache voveran sr 100 mg with amex, loose stools without visible blood spasms hamstring order genuine voveran sr, lasting less than two weeks. The common causes of acute watery diarrhea are viral, bacterial, and parasitic infections. The enteric pathogens causing this diarrhea in developing countries are largely the same that are encountered in developed countries, but their proportions are different. In general, bacterial pathogens are more important in countries with poor hygienic conditions. The most important causes of this diarrhea in developing countries are Rotavirus, Shigellae, entero toxigenic E. The most dangerous complication is dehydration that occurs when there is excessive loss of fluids and minerals (electrolytes) from the body. Dehydration is especially dangerous in infants and young children due to rapid body water turnover, high body water content and 13 relatively larger body surface. Moderate to severe dehydration may cause orthostatic hypotension with syncope (fainting upon standing due to a reduced volume of blood, which causes a drop in blood pressure upon standing), a diminished urine output, severe weakness, shock, kidney failure, confusion, acidosis (too much acid in the blood), and coma. Evidences showed that around 10 percent of diarrhoeal episodes in children under five years of age have visible blood in the stool. This 10 percent of episodes causes about 16 15 percent of diarrhea associated deaths in this age group. Other pathogens causing endemic dysentery in children include: Campylobacter jejuni, invasive strains of E. Entamoeba histolytica usually causes less than 2 percent of 16 episodes of bloody diarrhoea in children less than 5 years old. Persistent diarrhea is defined as diarrheal episodes of presumed infectious aetiology 3, 13 that have an unusually long duration and last at least 14 days. About 10 percent of diarrheas in children from developing countries become persistent, especially among those less than three years and more so among infants. Since persistent diarrhea is a major cause of malnutrition in the developing countries, even the milder, non fatal episodes contribute to the overall high mortality rates that are frequently associated with malnutrition in these countries. Several causes, probably in combination, include: infections with entero aggregative E. Chronic diarrhea: this term refers to diarrhea which is recurrent or long lasting due to mainly non infectious causes. Chronic diarrhea may be caused by gastrointestinal 3, 11 disease, may be secondary to systemic disease, may be psychogenic in nature. The prevalence is highest for children 6 11 months of age, remain at a high level among the one year old children, and 13, 17, 21, 22 decrease in the third and fourth years of life. Socio economic factors: Some studies have shown that the association between 13, 17, 19, 24 socio economic factors, such as poor housing, crowded conditions, low 13, 17, 24 income ; and higher rate of diarrhea was statistically significant. Water related factors: As diarrhea is acquired via contaminated water and foods, water related factors are very important determinants of diarrhea occurrence. Hygiene practices: Some studies have revealed that children not washing hand before 22, 29, 32, 33, 34 meals or after defecation, mothers not washing hands before feeding 22, 29, 32, 34 children or preparing foods, children eating with their hands rather than with 31 23 21, 30, 34 spoons, eating of cold leftovers, dirty feeding bottles and utensils, 17, 24, 33, 34 unhygienic domestic places (kitchen, living room, yard), unsafe food 34 23, 34 storage, presence of animals inside the house, presence of flies inside the house 34, were associated with risk of diarrhea morbidity in children. Breastfeeding: the literature on feeding practices and risk of diarrhea is extensive. In general, the morbidity of diarrhea is lowest in exclusively breast fed children; it is 13, 20, 35, 36, higher in partially breast fed children, and highest in fully weaned children 38 13, 30. A high concentration of specific antibodies, cells, and other mediators in breast milk reduces 13 the risk of diarrhea following colonization with entero pathogens. Malnutrition: the association between diarrhea and malnutrition is so common in low income societies that the concept of a vicious circle is appealing, with diarrhea 13, 39 leading to malnutrition and malnutrition predisposing to diarrhea. Children whose immune systems have been weakened by malnutrition are the most vulnerable to diarrhea. Diarrhea, especially persistent and chronic diarrhea, undermines nutritional status, resulting in malabsorption of nutrients or the inability to use nutrients properly to maintain health. A number of studies have reported higher incidence of diarrhea in 13, 39, 40 malnourished children. Due to innate or acquired immunodeficiency, patients are vulnerable to pathogens that 17 cause infectious diseases including diarrhea. Seasonal distribution: Seasonal patterns to childhood diarrhea have been noted in many tropical locations, where there are two definite seasonal peaks: the summer one, 8 associated with bacterial infections, and the winter one, related to viruses. In some studies diarrhea prevalence was found to be higher in the rainy season than in the dry 8, 42 season. During the dry seasons when rainwater and borehole water are less available, disinfecting drinking water from available surface sources may 29 substantially reduce illness. In some studies contamination was more prominent 22, 43, 44 during the rainy season. Teshima et al, the number of diarrhea patients in the first peak in April is sensitively correlated to climate elements in pre monsoon. Climate in pre monsoon influences the total number of diarrhea patients through the spring peak (April May) and the climate in August through October influences the autumn peak of patients. Meteorological elements play reverse role on the peak of spring and autumn diarrhea patient. There are also some researches reporting that a distinct increase of 46, 47, 48 diarrhea takes place in the years of El Nino. Tourists visiting foreign countries with warm climates and poor sanitation can acquire diarrhea by eating contaminated foods such as fruits, vegetables, seafood, raw meat, 8 water, and ice cubes. Eating habits: Eating with the hands; eating raw foods; or drinking unboiled water, may increase the risk of diarrhea. It is well known that diarrheal disease is one of the 18 leading causes of illness and death in young children in developing countries. Diarrhea accounts for 21% of all diseases causing deaths at below five years of age and causes 2. In addition, many time this number have long term, lasting effects on nutritional status, 2, 25, 49 growth, fitness, cognition, and school performance. It is believed that diarrhea have a significant impact on growth due to reduction in appetite, altered feeding practices 49 52 and decreased absorption of nutrients. For example, during infancy, boys who spent from 20% to less than 40% of their time with diarrhea were 5. At age of 1 4 years, with the same time spent with diarrhea, the 13 deficit on height was 2. Diarrhea during the first 6 months of life resulted in long term height deficits that were likely to be permanent. Similarly, Molbak 55 and Briend indicated that after 6 months of age, the effect of diarrhea on growth was transient due to catch up growth. Rehydration and its correction of any electrolyte imbalance is critical in the treatment of diarrhea. Not all diarrheal episodes in the developing countries are associated with dehydration and, consequently, do not require rehydration therapy. However, promotion of the basic concept that diarrhea and vomiting are likely to results in life threatening dehydration continues to be of great importance. This educational 3 promotion should be aimed at all levels from families to doctors. It has contributed substantially to reducing childhood deaths from diarrheal disease because it is 57 extremely effective in treating acute watery diarrhea. However, it is important to have a single acceptable formula that can be recommended and promoted worldwide. Symptomatic anti diarrheal drugs are usually not recommended for the treatment 3, 6 of acute diarrhea in children. Antimicrobials are not effective in uncomplicated acute diarrhea and their use should be discouraged. In contrast, antimicrobials are indicated in dysentery, cholera, typhoid fever and diarrhea caused by parasites, such 3, 8 as Giardia lamblia, Cyclospora and E. It recommends that breast feeding must not be interrupted; feeding according to age should be restarted as soon as clinical signs of dehydration disappear, and be continued even if severe diarrhea persists. Adequate dietary management during and after diarrheal disease is very important in order to reduce or prevent the damage of 20 intestinal functions induced by withholding foods; to prevent or decrease the nutritional damage caused by the disease; to shorten the duration of the disease; and to allow catch up growth and a return to good nutritional condition during 3 convalescence. A long term, sustainable solution to childhood diarrheal disease must combine treatment with actions to eliminate diarrheal disease through prevention. Feces Sanitation solution: latrine or toilet Fluids Fields Flies Fingers Hand washing Foods Family Figure1. It is estimated that 90% of the child diarrheal disease burden is the result of poor sanitation conditions and inadequate personal, household and community hygiene 60. Primary preventive interventions reduce environmental risk factors and high risk behaviors for whole communities by interrupting the disease transmission cycle 21 (Fig. For diarrheal disease this means promoting changes in hygiene behavior to protect people from ingesting diarrheal disease pathogens and providing sanitation solutions to protect the environment from fecal contamination. Torun, strategies for comprehensive prevention and control of diarrhea include: good personal and domestic hygiene; use of safe water; improved nutrition; immunization; and effective case management. Measles immunization: Of the existing vaccines, measles vaccine certainly has a potential in reducing mortality attributed to diarrheal disease since measles is 3 associated with diarrhea in some 20 % of the cases. Eight out of ten children who die do so at home, after having little or no contact with health facility staff. Besides, female education, improvements of socioeconomic status and vitamin A 3 supplementation may also play important roles in the prevention of diarrhea. Background Vietnam is located in South East Asia, between latitudes 9 and 23 degree north, and longitude 106 degree east. It borders the Gulf of Thailand, Gulf of Tonkin, and South China Sea, alongside China, Laos, and Cambodia. The country has an area of 329,560 square kilometres, stretching over 1,600km along the eastern coast of the 62, 63 Indochinese Peninsula. Among them, the Kinh ethnic group is the majority, making up 85 90 % of the population. Although the country is located in the tropical region, the climate is tropical only in central and southern Vietnam, with warm and humid weather all year round (22 o 35 C). Usually, the winter is also the dry season for the entire country, but the rains are highly 64 unpredictable owing to the influence of several monsoons. Vietnam is a poor country that has had to recover from the ravages of war and the rigidities of a centrally planned economy. Substantial progress was achieved from 1986 to 1996 in moving forward from an extremely low starting point growth averaged around 9% per year from 1993 to 1997. Growth then rose to 6% 62 to 7% in 2000 02 even against the background of global recession. Health care system in Vietnam Vietnam is divided into 4 administrative regions namely the North, the South, the Central and Highland, including 64 administrative provinces. Each province is divided into districts, and each district includes some communes. Ministry of Health is assigned to organize and manage health services all over the country. At local levels, provincial department of health, district medical centre and commune medical station are responsible for organizing, managing and providing health care services to the population in these areas. For health spending, Vietnam has achieved remarkable results for a country that has limited public resources. Progress in controlling vaccine preventable diseases, such as measles, diphtheria and 67 tetanus, has been rapid as well. Many new policy tools have been developed, including user fees, health insurance and health care funds for the poor. These tools all focus on the financing of health, but still fail to merge into a coherent health financing system. Limited budget also leads to many difficulties, especially the inadequacy of the check up system and shortage of hospital space. In most countries in the region, there is an average of 25 hospital beds for 10,000 people, whereas Vietnam only has 15 68 beds per 10,000 people. Due to high prices, many low income people cannot afford to access to these drugs. Diarrhea in Vietnam Crowded population, air and water pollution, poor sanitation, low hygienic practices and low socio economic status pose a serious threat to public health in Vietnam. Acute respiratory illness and diarrhea are leading causes of morbidity and mortality in children. However, the mortality could be underestimated due to the lack of surveillance information. Similarly, low morbidity and mortality of diarrhea in the period of 1990 1993 may be attributable to the weak surveillance system. In Vietnam, according to some studies, the most common pathogens causing diarrhea among children under five are rotavirus, E. The difference in the morbidity of diarrhea was insignificant between dry and rainy seasons nationwide, but in the north the higher prevalence of diarrhea has 70 been observed in the rainy season (May September). Over the world many studies have been conducted towards describing the epidemiology and risk factors for diarrheal disease among children less than five years of age. However, the local epidemiology of diarrhea in most rural areas of Vietnam has not been researched thoroughly. My study aimed to identify the most common pathogens of and local risk factors for diarrheal illness among children aged less than five years admitted to Dong Anh Hospital, Hanoi. Identification of pathogens and risk factors, and then recommendations of simple, immediate, and effective risk reduction measures would help local health care services to reduce morbidity and mortality due to diarrhea among young children in the area. Specific objectives To identify risk factors for and the most common pathogens of diarrhea among children less than five years old admitted to Dong Anh Hospital. Dong Anh is a suburban district locating in the north of Hanoi, at a distance of 40 kilometers from Hanoi city. Like many areas in Northern Vietnam, it has a hot and rainy season (from May to September), and a cold season (from October to April).
Preparation for emergencies in the offces of pediatricians and pediatric primary care providers spasms near temple order voveran sr no prescription. However yellow muscle relaxant 563 purchase voveran sr 100 mg overnight delivery, similarly low rates of medically signifcant wheezing and hospitalizations were observed in children 24 through 59 months of age regardless of the infuenza vaccine given muscle relaxant india cheap voveran sr 100 mg line. The proposed explanation for the low incidence of transmission is that the vaccine virus is shed for a shorter duration and in a much smaller quantity than are wild type strains muscle relaxant tizanidine quality 100mg voveran sr. Chemoprophylaxis should not be considered a substitute for immunization in most cases muscle relaxant trade names generic voveran sr 100mg online. However muscle relaxant glaucoma discount voveran sr 100mg without prescription, infuenza antiviral drugs are important adjuncts to infuenza immunization for control and prevention of infuenza disease. Because of high rates of resistance of 2009 pandemic infuenza A (H1N1), infuenza A (H3N2), and infuenza B strains to amantadine or rimantadine, oseltamivir, or zanamivir are recommended. However, recommendations for use of these drugs for chemoprophy laxis may vary by location and season, depending on susceptibility patterns. Providers should inform recipients of antiviral chemoprophylaxis that the risk of infuenza is low ered but still remains while taking medication, and susceptibility to infuenza returns when medication is discontinued. Manifestations are similar to those caused by other enteric protozoa (eg, Cryptosporidium and Cyclospora species) and can include abdominal pain, cramping, anorexia, nausea, vomiting, weight loss, and low grade fever. Infection results from ingestion of sporulated oocysts (eg, in contaminated food and water). Humans are the only known host for C belli and shed noninfective oocysts in feces. Under favorable conditions, sporula tion can be completed in 1 to 2 days and perhaps more quickly. Oocysts probably are resistant to most disinfectants and can remain viable for prolonged periods in a cool, moist environment. The incubation period is uncertain but ranges from 7 to 12 days in reported cases. This constraint under scores the utility of repeated stool examinations, sensitive recovery methods (eg, concen tration methods), and detection methods that highlight the organism (eg, oocysts stain bright red with modifed acid fast techniques and autofuoresce when viewed by ultra violet fuorescent microscopy). Pyrimethamine (plus leucovorin, to prevent myelosuppression) is an alternative treatment for people who cannot toler ate trimethoprim sulfamethoxazole. If untreated, approximately 20% of children may develop coronary artery abnormalities, including aneurysms. Approximately 80% of cases of Kawasaki disease occur in children younger than 5 years of age. The illness is characterized by fever and the following clinical features: (1) bilateral bulbar conjunctival injection with limbic sparing and without exudate; (2) erythematous mouth and pharynx, strawberry tongue, and red, cracked lips; (3) a polymorphous, generalized, erythema tous rash that can be morbilliform, maculopapular, or scarlatiniform or may resemble erythema multiforme; (4) changes in the peripheral extremities consisting of induration of the hands and feet with erythematous palms and soles, often with later periungual desquamation; and (5) acute, nonsuppurative, usually unilateral, cervical lymphadenopa thy with at least one node 1. For diagnosis of classic Kawasaki disease, patients should have fever for at least 5 days (or fever until the date of treatment if given before the ffth day of illness) and at least 4 of the above 5 features without alternative explanation for the fndings. Irritability, abdominal pain, diarrhea, and vomiting commonly are associated features. Other fndings include ure thritis with sterile pyuria (70% of cases), mild anterior uveitis (25%?50%), mild hepatic dysfunction (50%), arthritis or arthralgia (10%?20%), meningismus with cerebrospinal fuid pleocytosis (25%), pericardial effusion of at least 1 mm (less than 5%), gallbladder hydrops (less than 10%), and myocarditis manifested by congestive heart failure (less than 5%). A persistent resting tachycardia and the presence of an S3 gallop often are appre ciated. Rarely, Kawasaki disease can present with what appears to be septic shock? with need for intensive care; these children often have signifcant thrombocytopenia at admission. Group A streptococcal or Staphylococcus aureus toxic shock syndrome should be excluded in such cases. Incomplete Kawasaki disease can be diagnosed in febrile patients when fever plus fewer than 4 of the characteristic features are present. Patients with fewer than 4 of the characteristic features and who have additional fndings not listed above (eg, puru lent conjunctivitis) should not be considered to have incomplete Kawasaki disease. The proportion of children with Kawasaki disease with incomplete manifestations is higher among patients younger than 12 months of age. Infants with Kawasaki disease also have a higher risk of developing coronary artery aneurysms than do older children, making diagnosis and timely treatment especially important in this age group. Therefore, although labora tory fndings in Kawasaki disease are nonspecifc, they may prove useful in increasing or decreasing the likelihood of incomplete Kawasaki disease. If coronary artery ectasia or dilatation is evident, diagnosis can be made with certainty. A normal early echocardio graphic study is typical and does not exclude the diagnosis but may be useful in evaluation of patients with suspected incomplete Kawasaki disease. The average duration of fever in untreated Kawasaki disease is 10 days; however, fever can last 2 weeks or longer. After fever resolves, patients can remain anorectic and/or irritable for 2 to 3 weeks. During this phase, desquamation of the groin, fngers, and toes and fne desquamation of other areas may occur. Recurrent disease occurring months to years later develops in approximately 2% of patients. Coronary artery abnormalities can be demonstrated with 2 dimensional echocardiog raphy in 20% to 25% of patients who are not treated within 10 days of onset of fever. Characteristics suggesting disease other than Kawasaki disease include exudative conjunctivitis, exudative pharyngitis, discrete intraoral lesions, bullous or vesicular rash, or generalized adenopathy. Diagnosis, treatment and long term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Hispanic ethnic ity also has been associated with an increased risk of coronary artery aneurysms, which may be related to delayed diagnosis and treatment. Aneurysms of the coronary arteries have been demonstrated by echocardiography as early as 5 to 7 days after onset of illness but more typically occur between 1 and 4 weeks after onset of illness; their initial appear ance later than 6 weeks is uncommon. Aneurysms occurring in other medium sized arteries (eg, iliac, femoral, renal, and axillary vessels) are uncommon and generally do not occur in the absence of signifcant coronary abnormalities. In addition to coronary artery disease, carditis can involve the pericardium, myocardium, or endocar dium, and mitral or aortic regurgitation or both can develop. In children with mild coronary artery dilation or ectasia, coronary artery dimensions often return to baseline within 6 to 8 weeks after onset of disease. Approximately 50% of coronary aneurysms (fewer giant aneurysms) regress to normal luminal size within 1 to 2 years, although this process can be accompanied by development of coronary ste nosis. In addition, regression of aneurysm(s) may result in a poorly compliant, fbrotic vessel wall. The principal cause of death is myocardial infarction resulting from coronary artery occlu sion attributable to thrombosis or progressive stenosis. The relative risk of mortality is highest within 6 weeks of onset of symptoms, but myocardial infarction and sudden death can occur months to years after the acute episode. There is hypothetical concern that vasculitis of Kawasaki disease may predispose to premature coronary artery disease; longitudinal studies to test this hypothesis, however, have not been performed. Fifty percent of patients are younger than 2 years of age, and 80% are younger than 5 years of age; children older than 8 years of age less commonly develop the disease. In children younger than 6 months of age, the diagnosis often is delayed, because the symptom complex of Kawasaki disease is incomplete. The prevalence of coronary artery abnormalities is higher when diagnosis and treatment are delayed beyond the 10th day of illness. In the United States, 4000 to 5500 cases are estimated to occur each year; the incidence is highest in people of Asian ancestry. Kawasaki disease frst was described in Japan, where a pattern of endemic occurrence with superimposed epidemic outbreaks was recognized. A similar pattern of disease occurrence with occasional sharply defned community wide epidem ics has been recognized in North America and Hawaii. No evidence indicates person to person or common source spread, although the incidence is slightly higher in siblings of children with the disease. The diagnosis is established by fulfllment of the clinical criteria (see Clinical Manifestations, p 454) and clinical or labo ratory exclusion of other possible illnesses, such as staphylococcal or streptococcal toxin mediated disease; drug reactions (eg, Stevens Johnson syndrome); measles, adenovirus, parvovirus B19, or enterovirus infections; rickettsial exanthems; leptospirosis; systemic onset juvenile idiopathic arthritis; and reactive arthritis. Therapy should be initiated when the diagnosis is established or strongly suspected, optimally within the frst 10 days of illness. Once the acute phase has passed, therapy is directed at prevention of coronary artery thrombosis. A dose of 2 g/kg as a single dose, given over 10 to 12 hours, has been proven to reduce the risk of coronary artery aneurysm from 17% to 4%. Few complications occur from this regimen, but infusion reactions (fever, chills, hypotension) do occur, and drug induced aseptic meningitis is seen as a rare complication. A chest radiograph should be obtained before administration of infiximab to ensure that the patient does not have active tuberculosis (see Biologic Response Modifers, p 82). A tuber culin skin test should be placed, but treatment with infiximab should not be delayed awaiting results. The beneft and potential risks of systemic corticosteroids in treatment of Kawasaki disease are controversial. Aspirin is used for anti infammatory and antithrombotic actions, although aspirin alone does not decrease risk of coronary artery abnormalities. Aspirin is administered in doses of 80 to 100 mg/kg per day in 4 divided doses once the diagnosis is made. Children with acute Kawasaki disease have decreased aspirin absorption and increased clearance and rarely achieve therapeutic serum concentrations. Many centers change from high dose to low dose aspirin after the child has been afebrile for 48 to 72 hours. Other clinicians continue high dose aspirin therapy until day 14 of illness and 48 to 72 hours after fever cessation. Aspirin is discontinued if no coronary artery abnormalities have been detected by 6 to 8 weeks after onset of illness. Low dose aspirin therapy should be continued indefnitely for people in whom coronary artery abnormalities are present. In general, ibuprofen should be avoided in children with coronary aneurysms taking aspirin for its antiplatelet effects, because ibu profen antagonizes the platelet inhibition that is induced by aspirin. The child and house hold contacts should be given infuenza vaccine at the time of diagnosis of Kawasaki disease according to seasonal recommendations. Children also should be assessed during this time for arrhythmias, congestive heart failure, and valvular regurgitation. The care of patients with signifcant cardiac abnormalities should involve a pediatric cardiologist experienced in management of patients with Kawasaki disease and in assessing echocardiographic studies of coronary arteries in children. Long term management of Kawasaki disease should be based on the extent of coronary artery involvement. In patients with persistent moderately large coronary artery abnormalities that are not large enough to require anticoagulation, pro longed low dose aspirin and clopidogrel (1 mg/kg/day) are recommended in combina tion. Development of giant coronary artery aneurysms (diameter 8 mm or larger) usually requires addition of anticoagulant therapy, such as warfarin or low molecular weight heparin, to prevent thrombosis. Anticoagulation also sometimes is used in young infants with coronary artery aneurysms measuring less than 8 mm in diameter but for whom the size is equivalent to giant aneurysms when body surface area is considered. For example, a 3 month old infant with coronary arteries 6 or 7 mm in diameter often would be a candi date for anticoagulation. The schedule for administration of inactivated childhood vaccines should not be interrupted. K kingae may be a major cause of skeletal infections in children younger than 3 years of age. Pyogenic arthritis caused by K kingae generally is monoarticular, most commonly involving the knee, followed in frequency by the hip or ankle. Clinical manifestations of pyogenic arthritis are similar to manifestations associated with infection attributable to other bacterial pathogens in immunocompetent children, although a subacute course may be more common. Osteomyelitis caused by K kingae has clinical manifestations similar to Staphylococcus aureus osteomyelitis, but epiphy seal infection and a subacute course may be more common. Bacteremia can occur in previously healthy children and in children with preexisting chronic medical problems; some cases have occurred in adoles cents. In addition to fever, children with K kingae bacteremia frequently have concurrent fndings of respiratory or gastrointestinal tract disease. Of the 4 species in the genus Kingella, K kingae is the species most com monly associated with infection. The organism more frequently colonizes young children than adults and can be transmitted among chil dren in child care centers, generally without causing disease. Infection may be associated with preceding or concomitant stomatitis or upper respiratory tract illness. In patients with pyo genic arthritis and osteomyelitis, blood cultures often are negative for K kingae. Synovial fuid and bone aspirates from patients with suspected K kingae infection should be inoculated into Bactec, BacT/ Alert, or similar blood culture systems and held for at least 7 days to maximize recovery. Conventional and real time polymerase chain reaction methods have improved detection of K kingae in research studies. K kingae should be suspected in young children with culture negative skeletal infections. Penicillin is the drug of choice for treatment of invasive infections attributable to beta lactamase?negative strains of K kingae. Strains generally are susceptible to ampicillin sulbactam, aminoglycosides, ciprofoxacin, erythromycin, chloramphenicol, and oxacillin and are resistant to trim ethoprim, clindamycin, and vancomycin. Gentamicin in combi nation with penicillin can be useful for the initial treatment of endocarditis. Extended spectrum cephalosporins cefotaxime or ceftriaxone also may be used to treat endocarditis. Legionnaires disease varies in severity from mild to severe pneumonia characterized by fever, cough, and pro gressive respiratory distress.
Demonstrating strain relatedness will also provide insight as to whether the outbreaks were a single event or simultaneous independent outbreaks from several sources spasms near sternum discount voveran sr master card. Several risk factors have been associated with the development of nosocomial infection in newborns spasms sphincter of oddi generic voveran sr 100mg without prescription, the most important being birth weight muscle relaxant vitamins voveran sr 100mg line, immaturity of the immune system muscle relaxant equipment safe voveran sr 100mg, type and duration of invasive procedures 2410 muscle relaxant cheap voveran sr 100 mg on-line, and colonization by bacteria from hospital environment muscle relaxant 5658 purchase voveran sr 100 mg with visa. The outbreak investigation however revealed numerous lapses in hand hygiene practices. Running water is not always available and water is stored in plastic containers beneath the sink accessed using a common cup (Chapter 6, Figure 6. Patient to patient transmission in this study is certainly possible due to overcrowding with sharing of cots. Neonates in whom intestinal colonisation with Gram negative bacilli develops are a particularly important reservoir of Gram negative bacilli in the nursery; once colonised, infants may harbour antibiotic resistant hospital strains of Gram negative bacilli in their stool for up to a year or more. Many families have relatives in neighbouring countries (Senegal, Guinea Bissau) and there is a lot of cross border movement. Firstly, being a hospital based study, complete ascertainment of neonatal infection cases in the study area that did not make it to hospital was not possible. The majority of the population in the study area however, give birth in health facilities and home born neonates have good access to referral level care, thereby supporting a reasonable level of case ascertainment. The hospital environment is also a hot bed of infection transmission through unclean delivery and unhygienic practices. Given that over 90% of cases in this study were facility born and that all the pathogens in this study are known to be associated with neonatal nosocomial bloodstream infections177, 423 and outbreaks, infections in this study might all have been hospital acquired and not just those associated with the outbreaks. However, for non outbreak pathogens, this would be difficult to prove in the absence of environmental samples. Thirdly, there was non accurate measure of gestational age and deliberate selection bias against babies with lower birth weight, who were underrepresented in the sample. It is possible that the maternal flora changes substantially in the days following birth, progressively obscuring the source of causative pathogens with delayed bacterial culture, particularly among mothers of newborns with late onset infections. These were beyond the funding and time available for this PhD but are planned for part my post doctoral work. Inasmuch as the study findings may not be generalisable to all health facilities in the entire country, the multisite recruitment across the levels of care (teaching hospital, general hospital and major health centers) ensured good representation. In this setting, blood culture remains a valuable diagnostic tool despite being slow and offering modest tangible benefit for high mortality risk neonates, with results available before discharge or death for only 38% (35/91) of cases. An exploratory Pilot study of a novel molecular diagnostic tool, the TaqMan Array Card, demonstrated limited additional benefit of this technology over blood cultures. There is a need for improved infection control and antimicrobial stewardship to preserve limited antibiotic choices. Mention is also made of more general priority areas for neonatal infection research such as discovery of new biomarkers and development of more sensitive diagnostic tools. Programme Implications & Protocols (patient/community, hospital and national level). Infection prevention and control should encompass intrapartum care both in the hospital and at home. In this setting, poor neonatal inpatient outcomes are also related to operational factors including, but not limited to , lack of laboratory capacity, lack of appropriate antibiotics, shortage of intravenous fluids, over crowding of wards with sharing of cots and radiant warmer beds, as well as shortage of staff. This is an important first step in setting national newborn health targets and identifying priority areas for action. In spite of the increasing trend in 207 facility births in the Gambia, an estimated 37% of the 83, 000 annual births still take place at home with or without a skilled attendant. In this study, just over 90% of Cases were facility born implying that many home born babies do not make it to the hospital, and probably die at home unreported. Clean birth practices at home with no skilled attendant could reduce neonatal sepsis deaths by as much as 15%. In such settings, alcohol based hand gel may provide an alternative option that is bacteriocidal against a broad range of Gram negative and Gram positive aerobic bacteria, including those commonly associated with neonatal infections. A shift in the hospital based management of sick newborns with suspected infection is urgently needed to include routine blood cultures. Now that most births occur in facilities, a crucial opportunity to improve the collection of epidemiological data is through establishing a standardised facility based perinatal minimal dataset that will promote comparability of data with other units and regions. Extension of such a database to include other countries in the West African sub region will facilitate comparability of data and quality improvement collaborations. Epidemiological data draw attention to priorities to maximise progress towards improving newborn survival, but targets and data alone do not save lives; only changes in health systems and coverage of effective interventions do. Equally important is operations research and research that addresses political, economic, social, cultural, behavioural, and infrastructural issues involved in addressing mortality due to neonatal infections. Areas of focus relating to prevention and management of neonatal infections are listed in Table 8. Feasibility, cost and effectiveness of setting up newborn care corners in first referral units and district hospitals Feasibility and effectiveness of approaches to increase quality of care in hospitals using standardised protocols for management of newborn conditions. Implementation Facility based cluster randomised trials evaluating research the multi faceted hand hygiene promotion priorities programmes (alcohol based hand gel) Clinical trials of targeted interventions to interrupt contamination and transmission of pathogens. Well designed clinical trials evaluating new clinical diagnostic algorithms are needed. Such clinical algorithms would be based on a combination of clinical signs and host biomarkers that would discriminate between the neonatal infection syndromes sepsis, meningitis and pneumonia. Microfluidics is the study of the behaviour, precise control, and manipulation of fluids geometrically constrained to submillimetre (nanolitre or picolitre) channels. Single drops of blood, faeces, and saliva have all been tested with encouraging results. Infection control management is important, and interventions, isolated or as part of care bundles, need detailed, prospective evaluation in outbreak situations. Routine programmatic data require significant resources, including strengthening laboratory quality control and assurance measures, and use and appropriate interpretation of molecular diagnostics to detect pathogens (including viruses). Neonatal cause of death estimates for the early and late neonatal periods for 194 countries: 2000 2013. Neonatal severe bacterial infection impairment estimates in South Asia, sub Saharan Africa, and Latin America for 2010. Neonatal infections: Case definition and guidelines for data collection, analysis, and presentation of immunisation safety data. Clinical signs that predict severe illness in children under age 2 months: a multicentre study. What clinical signs best identify severe illness in young infants aged 0 59 days in developing countries? Effectiveness of home based management of newborn infections by community health workers in rural Bangladesh. Scientific rationale for study design of community based simplified antibiotic therapy trials in newborns and young infants with clinically diagnosed severe infections or fast breathing in South Asia and sub Saharan Africa. The Neonatal Research Network: History since 2003, future directions and challenges. Pathogens associated with sepsis in newborns and young infants in developing countries. Neontal sepsis many blood samples, few positive cultures: implications for improving antibiotic prescribing. Population based incidence and etiology of community acquired neonatal bacteremia in Mirzapur, Bangladesh: an observational study. Population based Incidence and Etiology of Community acquired Neonatal Viral Infections in Bangladesh: A Community based and Hospital based Surveillance Study. To tap or not to tap: high likelihood of meningitis without sepsis among very low birth weight infants. Neonatal meningitis: what is the correlation among cerebrospinal fluid cultures, blood cultures, and cerebrospinal fluid parameters? Utility of blood cultures in children admitted to hospital with community acquired pneumonia. Transthoracic lung aspiration for the aetiological diagnosis of pneumonia: 25 years of experience from the Gambia. Prevalence of Bloodstream Pathogens Is Higher in Neonatal Encephalopathy Cases vs. A novel diagnostic tool for detecting neonatal infections using multiplex polymerase chain reaction. Optimization of Multiple Pathogen Detection Using the TaqMan Array Card: Application for a Population Based Study of Neonatal Infection. Application of TaqMan low density arrays for simultaneous detection of multiple respiratory pathogens. A laboratory developed TaqMan Array Card for simultaneous detection of 19 enteropathogens. Association between stool enteropathogen quantity and disease in Tanzanian children using TaqMan array cards: a nested case control study. Interpreting complete blood counts soon after birth in newborns at risk for sepsis. Serum procalcitonin as a diagnostic marker for neonatal sepsis: a systematic review and meta analysis. The diagnostic and prognostic accuracy of five markers of serious bacterial infection in Malawian children with signs of severe infection. Novel biomarker combination improves the diagnosis of serious bacterial infections in Malawian children. Inflammatory mediators for the diagnosis and treatment of sepsis in early infancy. Reduction of unnecessary antibiotic therapy in newborn infants using interleukin 8 and C reactive protein as markers of bacterial infections. Biomarkers for diagnosis of neonatal infections: A systematic analysis of their potential as a point of care diagnostics. A ten year review of neonatal sepsis and comparison with the previous fifty year experience. Early onset neonatal sepsis in the era of widespread intrapartum chemoprophylaxis. Group B streptococcal disease: from trials and tribulations to triumph and trepidation. Group B Streptococcus and Escherichia coli infections in the intensive care nursery in the era of intrapartum antibiotic prophylaxis. Changing patterns in neonatal Escherichia coli sepsis and ampicillin resistance in the era of intrapartum antibiotic prophylaxis. Risk of early onset neonatal infection with maternal infection or colonization: a global systematic review and meta analysis. Maternal and neonatal colonization in Bangladesh: prevalences, etiologies and risk factors. Lower genital tract swabs in the prediction of intrauterine infection in preterm prelabour rupture of the membranes. Risk Factors for Early onset Group B Streptococcal Sepsis: Estimation of Odds Ratios by Critical Literature Review. The impact of water, sanitation and hygiene on key health and social outcomes: review of evidence. Early onset neonatal sepsis in Pakistan: a case control study of risk factors in a birth cohort. Effective interventions to reduce neonatal mortality and morbidity from perinatal infections. Global, regional, and national causes of under 5 mortality in 2000 15: an updated systematic analysis with implications for the Sustainable Development Goals. Estimates of possible severe bacterial infection in neonates in sub Saharan Africa, south Asia, and Latin America for 2012: a systematic review and meta analysis. Global Health Estimates 2015: Disease burden by Cause, Age, Sex, by Country and by Region, 2000 2015. Maternal and early onset neonatal bacterial sepsis: burden and strategies for prevention in sub Saharan Africa. Aetiology of community acquired neonatal sepsis in low and middle income countries. International cooperation to improve access to and sustain effectiveness of antimicrobials. Acute bacterial meningitis in children admitted to a rural Kenyan hospital: increasing antibiotic resistance and outcome. Clinical indicators of bacterial meningitis among neonates and young infants in rural Kenya. Invasive bacterial infections in neonates and young infants born outside hospital admitted to a rural hospital in Kenya. Acute bacterial meningitis among children, in Manhica, a rural area in Southern Mozambique. Neonatal septicaemia in a rural Nigerian hospital: aetiology, presentation and antibiotic sensitivity pattern. Risk factors for neonatal sepsis and perinatal death among infants enrolled in the prevention of perinatal sepsis trial, Soweto, South Africa. The clinical and bacteriogical spectrum of neonatal sepsis in a tertiary hospital in yaounde, cameroon. Clinical and bacteriological profile of neonatal bacterial infection at Laquintinie Hospital, Douala, Cameroon. Predominance of multi drug resistant Klebsiella pneumonia and other gram negative bacteria in neonatal sepsis in Equatorial Guinea. Bacterial profile and antimicrobial susceptibility pattern in septicemia suspected patients attending Gondar University Hospital, Northwest Ethiopia.
Cost of voveran sr. Binaural Beats: "Muscle Relaxant" - Pain Relief Recovery Rejuvenate Pure Tone.
References
- Laurenzi GA, Potter RT, Kass EH. Bacteriologic flora of the lower respiratory tract. N Engl J Med 1961; 265: 1273-1278.
- Katz JN, et al. Safety of reduced anti-thrombotic strategies in HeartMate II patients: a one-year analysis of the US-TRACE Study. J Heart Lung Transplant. 2015;34(12):1542-1548.
- Kawinska A, Dumont M, Selmaoui B, Paquet J, Carrier J. Are modifications of melatonin circadian rhythm in the middle years of life related to habitual patterns of light exposure? J Biol Rhythms 2005;20(5):451-60.
- Stengel D, Rademacher G, Ekkernkamp A, et al: Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma, Cochrane Database Syst Rev (9):CD004446, 2015.
- Dillon BE, Gurbuz C, Zimmern PE: Long term results after complication of iprophylactici suburethral tape placement, Can J Urol 19:6424n6430, 2012.
- Jha A, Duncan B, Bates D: Fatigue, Sleepiness and Medical Errors. Making Health Care Safer: A Critical Analysis of Patient Safety Practices, Evidence Report/Technology Assessment: Number 43 [AHRQ Publication No. 01-E058]. Rockville, MD, 2001, Agency for Healthcare Research and Quality. 173.
- Gattinoni L, Brazzi L, Pelosi P, et al. A trial of goal-oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995;333:1025-1032.
- Nucci M, Anaissie EJ, Queiroz-Telles F, et al. Outcome predictors of 84 patients with hematologic malignancies and Fusarium infection. Cancer 2003; 98(2):315-9.